Preventing Vascular Dementia: What You Must Know Before It’s Too Late
Worried about dementia? You’re not alone. Whether you’re noticing early warning signs in yourself or watching a loved one struggle with memory loss and confusion, it’s natural to fear what might come next. But here’s the truth most people never hear: vascular dementia is largely preventable—if you know what to look for and take action early. Taking action early is essential. If you wait for the diagnosis, the process has already been going on for 10-20 years.
In this comprehensive guide, we’ll walk you through:
- What causes vascular dementia and how it different from Alzheimer’s
- The silent warning signs you must not ignore
- The critical lab markers and imaging tests you should be getting
- Why your blood sugar, insulin, gut health, and sleep quality matter more than you think
- A practical, proactive roadmap to reduce your risk of dementia starting now
What Is Vascular Dementia?
Vascular dementia is the second most common type of dementia, just behind Alzheimer’s. Unlike Alzheimer’s, which primarily involves beta-amyloid plaques, vascular dementia is caused by poor blood flow to the brain—often due to cardiovascular issues like high blood pressure, diabetes, or stroke.
And here’s the shocking part: up to 44% of dementia cases in people over 80 are directly linked to vascular problems. That means nearly half of those cases might have been avoided.
It should be noted that you can have both vascular and Alzheimer’s at the same time; it doesn’t have to be one or the other. Understanding the difference between vascular dementia and Alzheimer’s can help with more targeted treatment.
Why Neuroplasticity Matters in POTS Recovery
Neuroplasticity is your brain’s ability to change, adapt, and form new connections based on the information it receives. And it can go one of two ways:
- Positive neuroplasticity creates new, healthy patterns.
- Negative neuroplasticity reinforces dysfunctional loops that keep your symptoms alive.
When you’re living with POTS, your brain and nervous system have learned to operate in a dysregulated state. You didn’t choose this, but the longer it goes on, the more deeply those patterns get wired in.
This is why surface-level treatments often fail. They don’t address the why. They don’t rewire the brain. And they don’t promote positive neuroplasticity, which is the only way real, long-term healing happens.
The Most Common Misconception: “It’s Just Genetics”
Many people believe that if dementia runs in their family, it’s only a matter of time. But genetics is not destiny. Lifestyle factors like diet, blood sugar stability, inflammation, sleep quality, and gut health can play a much bigger role in your actual risk.
Yes, having a parent or sibling with dementia increases your risk—but the majority of people with dementia do not have a strong genetic predisposition. You often share lifestyle habits, exposures, and diet with family, which makes those elements key targets for vascular dementia prevention.
Early Signs of Vascular Dementia (and When to Worry)
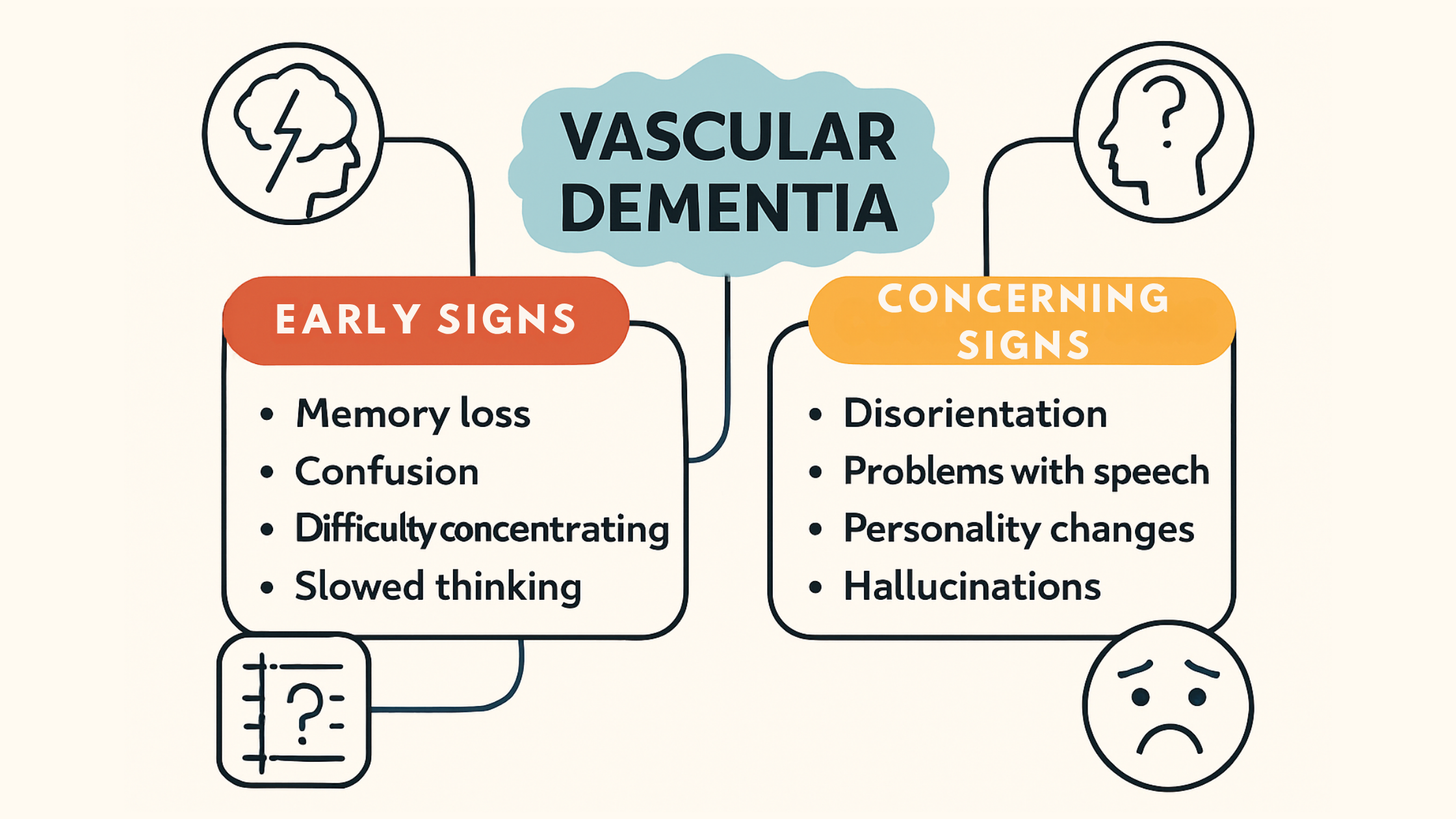
Know the signs of vascular dementia
Waiting until dementia symptoms are “bad enough” to take action is a dangerous gamble. The reality is, physiological changes in the brain start 10–20 years before diagnosis.
Subtle early signs of vascular dementia to watch for:
- Misplacing items more frequently
- Walking into rooms and forgetting why
- Trouble recalling recent events or conversations
- Struggling to follow multi-step instructions
- Word-finding difficulties in conversation
- Mild depression, anxiety, or new mood changes
More Concerning Signs (Often Seen Later):
- Getting lost while driving familiar routes
- Inability to manage finances or household tasks
- Hallucinations or delusions
- Asking the same question repeatedly
The Vascular-Dementia Connection: Why Cardiovascular Health Is Brain Health
Think of your brain like a high-performance engine. It needs optimal blood, oxygen, and nutrients to function. When your heart and blood vessels are compromised, your brain suffers. When everything is firing optimally, you feel sharp and clear, and your memory will outlast your physical body. In order to do this the brain needs blood, oxygen, and nutrients to function properly. When your heart and blood vessels are compromised, your brain suffers—slowly and silently.
Vascular dementia risk factors include:
- High blood pressure
- Obesity
- Insulin resistance
- Diabetes or prediabetes
- Heart Disease or Coronary Artery Disease
- Stroke
- Sleep apnea
- Sedentary lifestyle
For each risk factor that someone has, the likelihood of developing vascular dementia goes up.
The Most Overlooked Lab Tests That Predict Your Brain’s Future
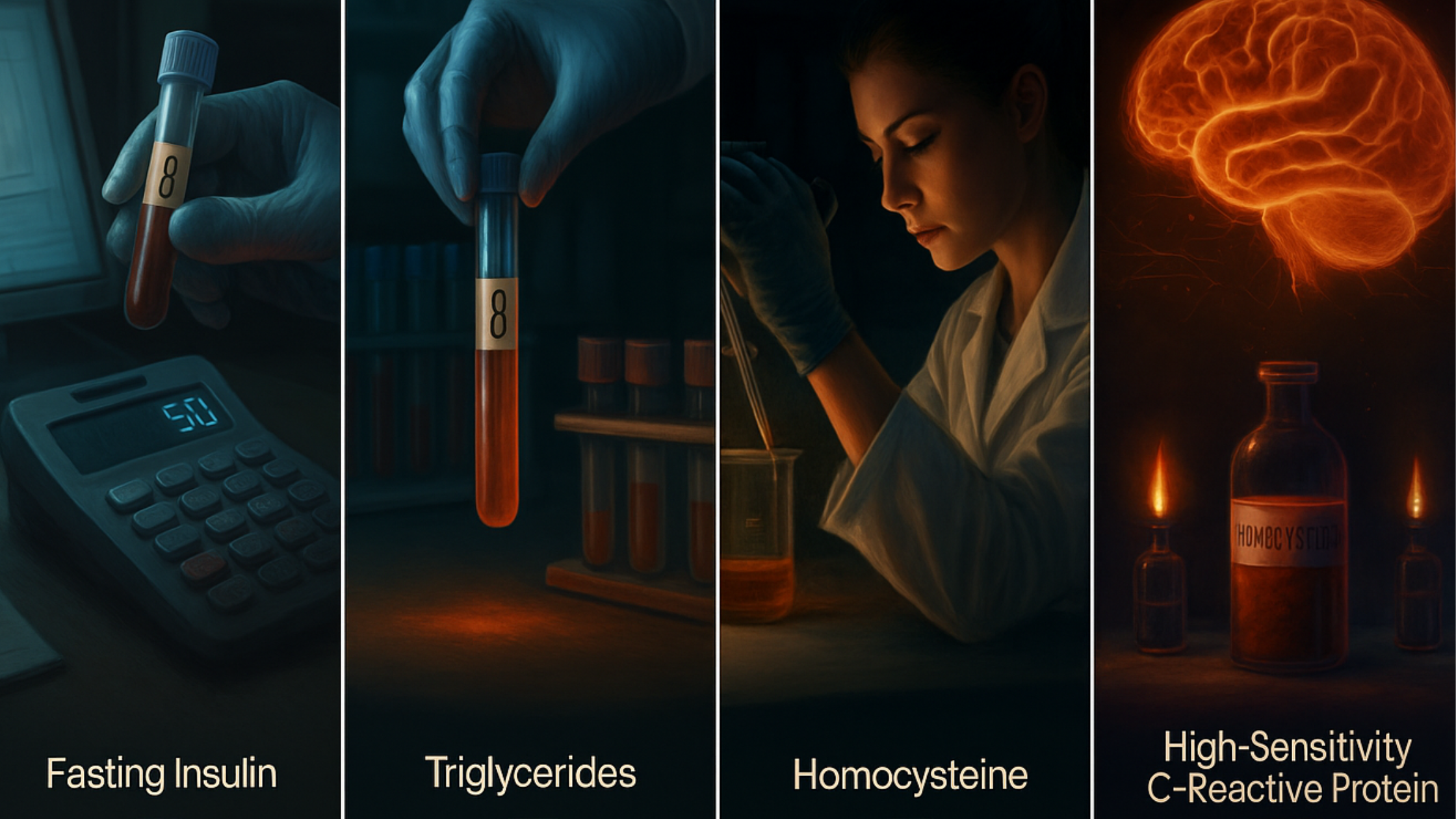
Essential lab markers for understanding metabolic and brain health
If you only rely on basic annual checkups, you’re likely missing critical data that could help you prevent cognitive decline. While there are numerous tests and studies that could be performed, here are the lab markers that matter most:
1. Fasting Blood Sugar
- Ideal: In the 80s
- Even “normal” results in the 90s can increase your dementia risk over time.
2. Hemoglobin A1c (HbA1c)
- Ideal: Around 5.0%
- “Normal” is often considered anything under 5.7%, but the lower the better. There is no harm in having the number lower, but the higher it is, the greater the risk.
3. Fasting Insulin
- Ideal: Under 8 (some experts prefer under 5)
- High fasting insulin is an early sign of insulin resistance. This will usually be off before blood sugar changes.
4. C-Peptide
- Ideal: Under 2.5
- Stable marker that reflects insulin sensitivity. The higher the number, the more likely there is insulin resistance.
5. Triglycerides
- Ideal: Under 75
- Triglycerides store unused sugar as fat—a hidden marker of metabolic imbalance.
6. Homocysteine
- Ideal: Between 5 and 8
- Levels over 10 are associated with vascular damage and higher dementia risk.
7. High-Sensitivity C-Reactive Protein (hs-CRP)
- Indicates systemic inflammation, a key driver of both heart disease and brain decline.
You may have noticed that many of these recommended lab values are different from what a standard lab considers normal. Remember, standard lab ranges include a lot of sick people and don’t reflect a healthy population.
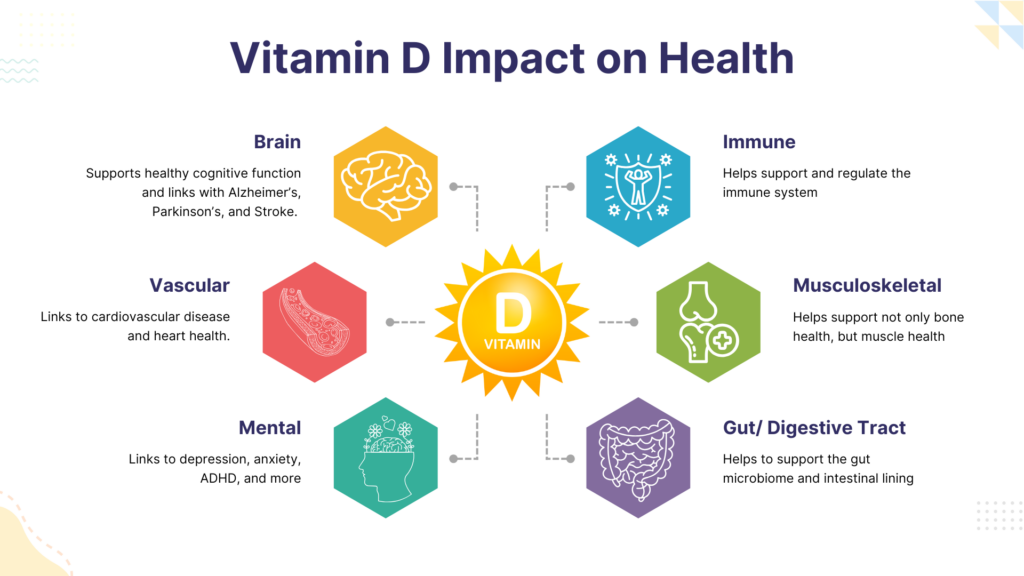
Don’t Ignore Gut Health: The Brain-Gut Connection Is Real
How does gut health affect the brain? Did you know your gut microbiome can influence your brain health? is a growing area of research. Imbalances in gut bacteria can drive inflammation and cognitive issues, even if digestion feels fine.
What to look for:
- Gut diversity, beneficial metabolites like butyrate
- Inflammatory markers like lipopolysaccharide
Can poor sleep cause dementia? Absolutely.
Pro tip: You don’t need diarrhea or constipation to have gut dysfunction. Fatigue, brain fog, anxiety, and autoimmunity are often tied to hidden gut issues.
Imaging: What Your Heart and Brain Are Trying to Tell You
1. Coronary Artery Calcium Score (CAC)
- A CT scan that measures calcified plaque in your arteries
- Reveals early signs of cardiovascular disease before symptoms appear
- Suggested starting around age 30 and every 5 years thereafteras long as it’s normal.
2. MRI Brain Scan
- Look for phrases like
- “White matter hyperintensities”
- “Chronic microvascular ischemia”
- “White matter hyperintensities”
- These indicate compromised blood flow to the brain—but are often dismissed as “normal aging.”
- Even normal imaging doesn’t mean everything is fine; it simply means it didn’t detect what the imaging is made to detect.
Tip: Always ask for a copy of your imaging report—and read it yourself or review it with a specialist. We routinely see these findings on MRIs that other providers have ordered, and patients state no one has ever told them about the findings.
Sleep: The Hidden Key to Preventing Dementia
If you snore, wake up unrefreshed, or feel tired during the day—you might have obstructive sleep apnea. Left untreated, this can raise blood pressure, worsen insulin resistance, and skyrocket your dementia risk.
Why Sleep Matters:
- It’s when your brain flushes out toxins via the glymphatic system
- Poor sleep = more inflammation = more cognitive decline
Move More, Think Better: Exercise and Brain Health
Physical activity is one of the most well-researched tools for reducing the risk of all types of dementia—including vascular dementia.
Aim for:
- 150 minutes per week of moderate cardio
- Strength training 2-3x/week.
- Daily walking and stretching to reduce sedentary time
You won’t always feel like exercising, and that’s okay, but keep your focus on why you are doing it. You are doing it to prevent dementia and not necessarily to become insanely ripped.
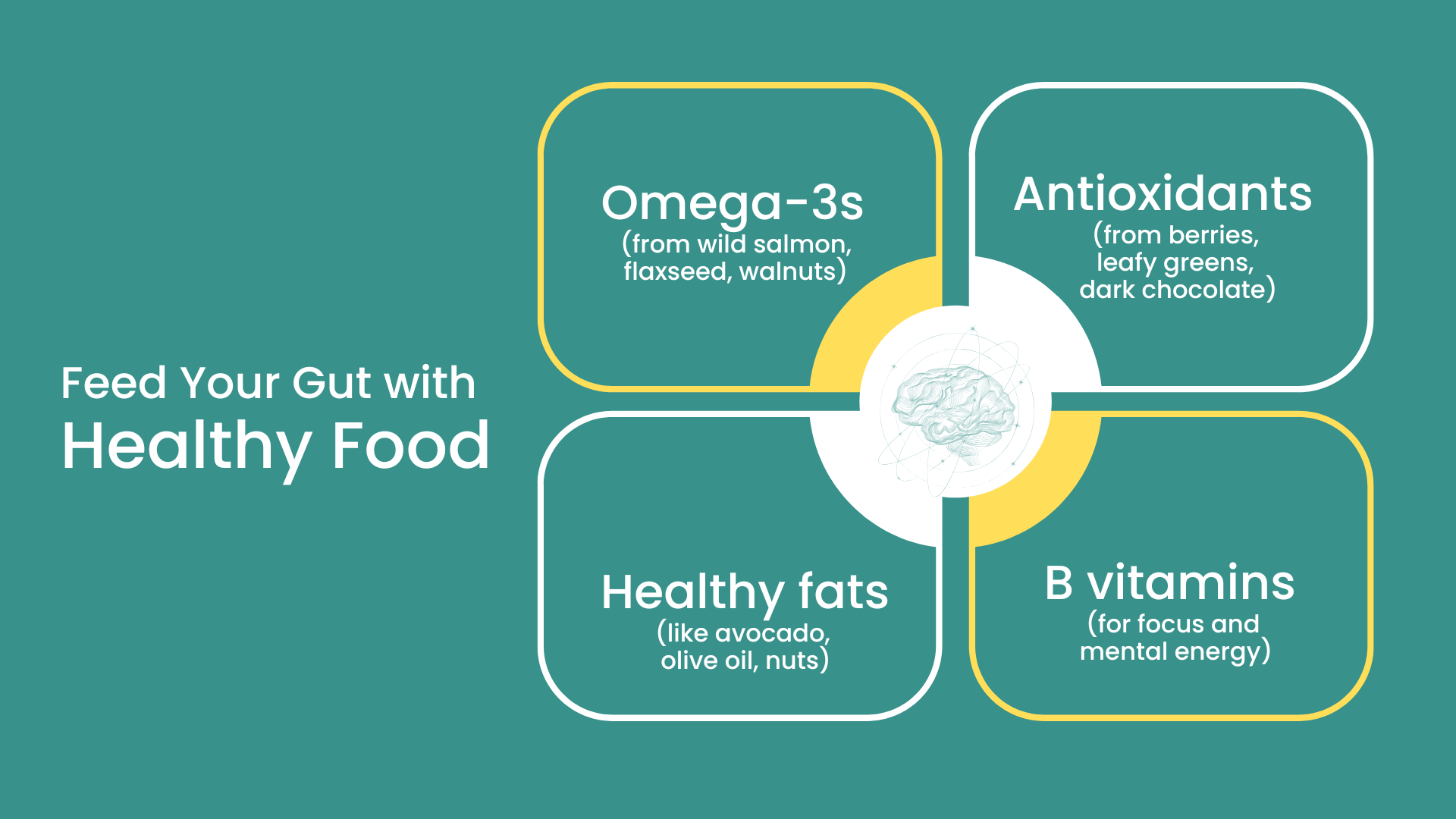
Diet and Lifestyle: What You Eat Today Shapes Your Brain Tomorrow
Healthy VS Unhealty Diet
Ultra-processed foods inflame your gut, spike your blood sugar, and damage your cardiovascular system. It’s a recipe for brain decline.
Build Your Plate With:
- 50% colorful, fiber-rich vegetables
- 30–35% healthy proteins and fats (grass-fed beef, wild-caught fish, avocado, nuts)
- 10–15% low-glycemic carbs (berries, legumes)
Avoid:
- Packaged, processed, microwaveable meals
- Sugary snacks, sodas, and refined carbs
- Chronic blood sugar spikes and crashes
- Fruit juices
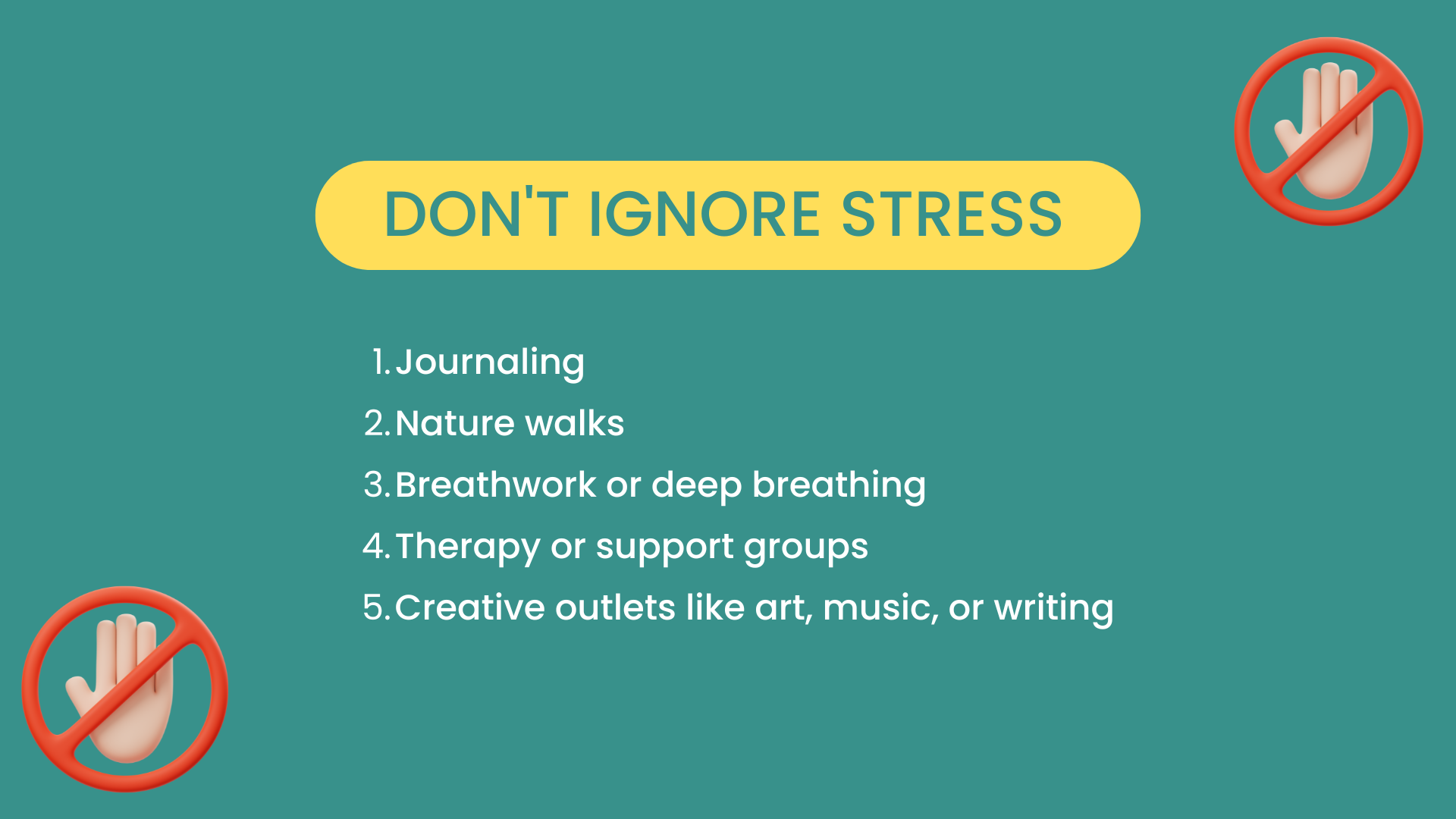
Hormones and Stress: The Silent Saboteurs
Low testosterone or estrogen? Chronically stressed? Both of these increase your risk.
- Hormones play a role in maintaining blood vessel health and brain resilience.
- Stress, whether emotional or physiological, activates inflammatory responses in the brain, damaging key memory centers like the hippocampus.
- Chronic stress can also prevent your body from producing sex hormones—testosterone, estrogen, and progesterone—in the appropriate amounts.
Stress management is not optional—it’s brain-saving.
When was the last time you did something you truly enjoyed? Optimizing health involves getting off the hamster wheel of life and allowing the brain and body time to heal and recover.
Final Thoughts: It’s Not Just About Getting Old
Watching someone forget your name… forgetting how to drive… or struggling to finish a sentence—these things don’t have to be your future.
Yes, some risk factors are out of your control. But the majority of vascular dementia risk comes from lifestyle choices made day in and day out.
You can start now by asking yourself:
- How well am I sleeping?
- Am I eating for blood sugar stability and gut health?
- When was my last in-depth lab work or brain scan?
- How often do I move, socialize, laugh, and learn?
The best time to start preventing dementia was 10 years ago. The second best time is today.
Ready to Take Control of Your Brain Health?
At our Peak Brain and Body Concussion treatment center located at 2404 Creel Ln, Suite 101, Wesley Chapel, FL 33544, we specialize in early detection and proactive prevention.
We use advanced diagnostics including laser therapy for brain injury to help support recovery and brain function. Led by Dr. Spencer Zimmerman, also known as Dr. Zimmerman, our team delivers personalized protocols tailored to your unique needs.
Looking for a new treatment for vascular dementia? You don’t have to wait for symptoms to worsen.
👉 Schedule your Brain-Body Insight Session today and take the first step toward preserving your memory and vitality.
ICD-10 Code Note: The vascular dementia ICD 10 code is F01.50 (without behavioral disturbance) and F01.51 (with behavioral disturbance) for clinical reference.