What Causes Brain Fog? A Systems-Based Look at the 6 Root Causes
If you’ve ever found yourself walking into a room and forgetting why, struggling to find the right words during a conversation, or feeling like your brain is stuck in a haze—you’re not alone.
You are likely dealing with brain fog and have probably thought what causes brain fog causes?
“Brain fog” is one of the most common complaints we hear in our clinic, Peak Brain and Body—a functional medicine and functional neurology clinic in Wesley Chapel. Some know it’s an issue they want addressed, but others aren’t sure if it’s just a normal part of aging. Yet despite how widespread it is, it’s often dismissed, misunderstood, or chalked up to aging, stress, or hormones. But here’s the truth:
Brain fog is not “just in your head.” It’s your body’s way of telling you that something deeper is off, but it’s non-specific.
In this article, we’re going to explore six major systems in the body that can cause or contribute to brain fog—many of which are often overlooked by conventional healthcare. If you’re someone who’s tried supplements, changed your diet, and still feels “off,” this deep dive is for you.
You may also watch it here: https://www.youtube.com/live/YDeuV-rS8I0
What Is Brain Fog?
First things first: brain fog isn’t a diagnosis. It’s a symptom – a signal that something in your body is out of balance. It might show up as:
-
Difficulty focusing or concentrating
-
Forgetting common words or losing your train of thought mid-sentence
-
Feeling mentally fatigued even after sleeping well (especially if you experience sleep deprivation)
-
Zoning out or spacing out during the day
-
A sense that your brain is “in a cloud”
And while it’s common, it’s not always normal – especially when it starts affecting your daily life, your relationships, and your ability to work and connect with others.
Now let’s look at why brain fog happens and what your body may be trying to tell you. Remember, brain fog is always a neurological symptom, but it may not always be due to poor brain health and may be the result of problems in other parts of the body like Gut Health, thyroid imbalance brain fog, insulin resistance brain fog symptoms, or even post-COVID gut brain fog.
So, what causes brain fog?
The Six Body Systems That Can Cause Brain Fog
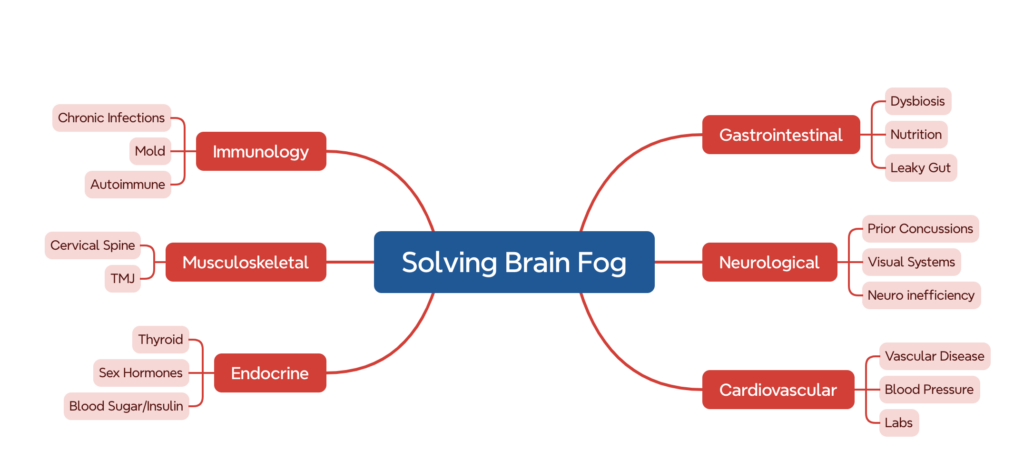
Graphic Representation of Brain Fog
1. Gastrointestinal (Gut) Health and Brain Fog
Your Gut Health and your brain are intimately connected through what scientists call the gut-brain axis. The bacteria in your gut produce neurotransmitters, influence inflammation levels through metabolites known as short chain fatty acids, and communicate directly with your nervous system.
When something is off in the gut, your brain may be impacted.
Common gut-related contributors to brain fog:
-
Dysbiosis: An imbalance in gut bacteria. You may have too many harmful bacteria or too few beneficial ones. This disrupts digestion, nutrient absorption, and produces inflammatory byproducts that can affect brain function.
-
Leaky Gut (Intestinal Permeability): When the gut lining becomes too porous, it allows toxins, food particles, and bacteria to enter the bloodstream and trigger systemic inflammation, including in the brain.
-
Processed Foods & Inflammatory Diets: Diets high in sugar, refined carbs, and additives fuel inflammation in both the gut and brain. For some, over time this leads to decreased mental clarity. For others, they may notice changes in brain function minutes or hours after eating foods or drinking certain things.
Some individuals experience post-COVID gut brain fog, where lingering gut inflammation and immune dysregulation cloud cognitive function.
How to address it:
-
Track your food intake for 7 days. Cut out ultra-processed foods and added sugars as a good starting point.
-
Consider an elimination diet or Paleo-style eating plan (vegetables, high-quality proteins, healthy fats). Track how you feel with the dietary changes. If you try to reintroduce foods and notice a negative shift, it’s best to avoid those items.
-
If you’ve cleaned up your nutrition and symptoms persist, stool testing can evaluate your microbiome and identify dysbiosis, pathogens, or leaky gut markers. This allows you to receive a specific treatment designed for you—often including psychobiotics for brain fog to support neuro-immune function.
2. Neurological Function and Brain Fog
Brain fog is a neurological symptom, meaning something is disrupting the way your brain functions. It could be:
-
Old concussions (even ones from years ago). In our experience 90% of individuals who are still struggling with concussion issues have no clue it’s what is keeping them stuck.
-
Neurological inefficiency (your brain is working too hard to complete simple tasks)
-
Visual processing—the brain has to take in an enormous amount of information, and this can be taxing on the brain. Problems with eye movement function, such as gaze fixation, pursuits, saccades, and vergence, can lead to brain fog.
Your brain uses more energy than any other organ. When it becomes inefficient—whether due to an old injury, eye strain, or abnormal sensory input—it starts to feel foggy.
Brain Testing & evaluation:
-
Computerized eye movement testing (video oculography) evaluates gaze fixation, saccades, and pursuits. Nearly 99% of our patients have never had this test performed. It’s off in upwards of 75% of the individuals we see and is a big piece of their inability to get the results they want until it gets addressed—highlighting the need for functional neurology treatment.
-
Balance testing and qEEG (quantitative EEG) identify areas of neurological inefficiency.
-
A thorough history can reveal concussions that may have been overlooked or dismissed.
Addressing neurological function isn’t just for athletes—it’s often the missing piece in brain fog recovery for those who have tried everything else, like hormones, B-vitamins, thyroid interventions, and other therapies.
3. Cardiovascular Health and Brain Fog
Your brain relies on constant, efficient blood flow to function. If your cardiovascular system isn’t working well, your brain may be under-supplied with oxygen and nutrients.
Subtle cardiovascular contributors to brain fog include:
-
High blood pressure or undiagnosed hypertension
-
Hypotension as seen in dysautonomia
-
Elevated triglycerides or cholesterol
-
Inflammatory markers like homocysteine
-
Lipoprotein(a) and ApoB (which increase your risk of plaque buildup)
-
Low omega-3 fatty acid intake
How to evaluate it:
-
Full lipid panel, including ApoB and Lipoprotein(a)
-
Homocysteine levels
-
Omega-3 to omega-6 ratio
-
Coronary artery calcium (CAC) scan to assess plaque buildup
Even if you feel “fine,” silent cardiovascular issues could be stealing your brain’s clarity. It takes years for cardiovascular trouble to show up. Prevention is key for lasting brain fog recovery.
4. Immune System & Chronic Inflammation Contributing to Brain Fog
Chronic Inflammation is one of the most common underlying causes of brain fog. When your immune system is out of balance, your brain function can suffer. Many factors already discussed—like gut dysfunction and hormonal shifts—also drive immune changes.
Major immune contributors to brain fog:
-
Chronic infections (Epstein-Barr virus, herpes virus, Candida, gut infections without fevers)
-
Mold exposure (inflammatory reactions in sensitive individuals)
-
Autoimmunity (Hashimoto’s, lupus, MS, rheumatoid arthritis, Crohn’s, ulcerative colitis—all associated with brain fog symptoms)
How to evaluate it:
-
Immune testing for mold (IgG, IgE to mycotoxins)
-
ANA panel and tissue-specific autoimmune markers based on symptoms/history
-
Lab testing for chronic infections via blood or stool
Autoimmunity is a spectrum. Early detection provides the best opportunity for healing. Identifying immune dysfunction early supports more effective brain fog recovery.
5. Musculoskeletal System and Brain Fog
Tension, misalignment, or dysfunction in the muscles and joints of your upper spine, neck, or jaw can contribute to pain and brain fog.
Key physical contributors:
-
TMJ dysfunction (tenderness or tightness in the jaw)
-
Neck misalignment or tension
-
Poor posture from screen use
While chiropractic care can help in some cases, musculoskeletal issues are rarely the only cause of brain fog. If you also have neck pain or headaches, it should be evaluated—especially during a brain fog recovery journey.
Self-check: Press gently where your jaw hinges, just below your temples. If it’s tender, you may benefit from TMJ therapy or manual work on those muscles.
6. Endocrine System (Hormones & Blood Sugar) and Brain Fog
Hormonal imbalances and blood sugar instability are major drivers of brain fog.
Top endocrine contributors:
-
Thyroid dysfunction—when slow, it often causes thyroid imbalance brain fog. The most common underlying cause is Hashimoto’s.
-
Sex hormone imbalance (estrogen, progesterone, testosterone)—these impact immune and brain health.
-
Insulin resistance brain fog symptoms—even if you’re not diabetic, blood sugar spikes or dips can cloud your brain.
Lab work to ask for:
-
Full thyroid panel (TSH, Free T3/T4, Total T3/T4, Thyroid antibodies)
-
Sex hormones (Free/total testosterone, estradiol, progesterone, total estrogen)
-
Blood sugar labs (Fasting glucose, insulin, C-peptide, triglycerides, OGTT)
If you feel tired or foggy after eating, your blood sugar may be on a roller coaster. Tracking how food affects energy is a key part of brain fog recovery.
Peak Brain and Body Treatment For Brain Fog
If you’ve seen multiple providers and still feel foggy, it’s not your fault. Most primary care visits are rushed. Most specialists only focus on one system.
The reality is: brain fog is usually not caused by just one thing. It’s a sign that your body is out of balance in multiple areas.
That’s why at Peak Brain and Body in Wesley Chapel, we use an integrated, systems-based approach to uncover the unique combination of factors affecting each patient—including Gut Health, immune, neurological, metabolic, and hormonal contributors—to guide your brain fog recovery.
We look at both brain and body health, not one or the other. This allows us to identify the pieces of your puzzle contributing to brain fog.
You Deserve to Feel Sharp Again
If brain fog is interfering with your work, your relationships, or your sense of self, don’t ignore it.
The earlier you uncover the root causes, the sooner you can start reversing the damage. And yes—for most people, brain fog recovery is possible. You won’t have to wonder any longer what causes brain fog.
Individuals routinely turn to Peak Brain and Body in Wesley Chapel as a trusted center for Functional Medicine and Functional Neurology to find answers to chronic and complex symptoms and conditions.
If you’re ready to stop guessing and start healing, we’re here to help.
About Dr. Spencer Zimmerman
Dr. Zimmerman is a dual-licensed Nurse Practitioner and Chiropractor—and is the only dual-licensed provider in Florida with advanced training in Functional Neurology, Functional Medicine, and Peptide Therapy. He is the best-selling author of Brain Reset: 7 Steps to a Healthier Brain and the founder of Peak Brain and Body in Wesley Chapel, FL.