Dysautonomia and POTS Treatment| Peak Brain and Body | Tampa and Wesley Chapel, FL
Dysautonomia, POTS, and Chronic Fatigue – Why You Have Dizziness, Headaches, and Other Common Symptoms
This may be the first time you’ve heard the phrase Postural Orthostatic Tachycardia Syndrome (POTS Syndrome), or you’ve been battling this condition for years and are struggling to find answers. Dr. Zimmerman at Peak Brain and Body has helped many in Tampa, FL, and beyond get their lives back through advanced testing and treatment for POTS and autonomic dysautonomia.
This blog is going to provide insight into not only what POTS and chronic fatigue are but also what dysautonomia is, why treating it as a cardiovascular-based condition fails so many, and what real solutions look like.
There is also a YouTube version of this: watch here
What Is POTS?
POTS is a form of dysautonomia, meaning it involves dysfunction in the autonomic nervous system—the system responsible for controlling involuntary functions like heart rate, blood pressure, digestion, and temperature regulation. It primarily affects women, with an estimated 80% of cases occurring in females.
The defining characteristic of POTS is an excessive increase in heart rate (by 30 beats per minute for adults, or 40 beats per minute for teens) within 10 minutes of standing, without a significant drop in blood pressure. If blood pressure does drop significantly, then it falls under broader dysautonomia causes rather than POTS specifically.
POTS vs. Dysautonomia: What’s the Difference?
Dysautonomia is a broader term referring to dysfunction in the autonomic nervous system. POTS is a specific subtype of dysautonomia, characterized by increased heart rate upon standing without major blood pressure drops. If blood pressure does drop significantly, then the condition falls under categories like orthostatic hypotension rather than POTS.
While all POTS patients have dysautonomia, not all dysautonomia patients have POTS. Think of it like this: If dysautonomia were a car brand, POTS would be one specific model. Understanding this distinction is crucial because treatment approaches will differ when you see a traditional medical provider. It doesn’t matter as much when we look at non-traditional approaches, which you’ll understand a lot more as you progress through this article.
Who Gets POTS and Why?
Over 3 million Americans are estimated to have dysautonomia POTS, and cases have skyrocketed, especially following COVID-19. It is important to note that it existed before COVID-19, but it wasn’t a routinely accepted diagnosis. This led to many individuals who’ve dealt with it in the past not receiving a diagnosis. While COVID-19 infection is known to cause POTS or dysautonomia, it’s not the only thing. Other known triggers include:
- Viral infections (including flu and COVID-19)
- Concussions and brain injuries (including mild concussions that were dismissed)
- Autoimmune conditions (POTS can be an autoimmune-driven disorder)
- Chronic migraines (which can be both a cause and an effect of POTS)
- Surgery and prolonged bed rest
- Mast cell activation syndrome (MCAS)
- Vaccine side effects
- Hormonal shifts (such as menstruation and perimenopause)
- Genetic disorders like Ehlers-Danlos Syndrome (EDS) (particularly hypermobile EDS)
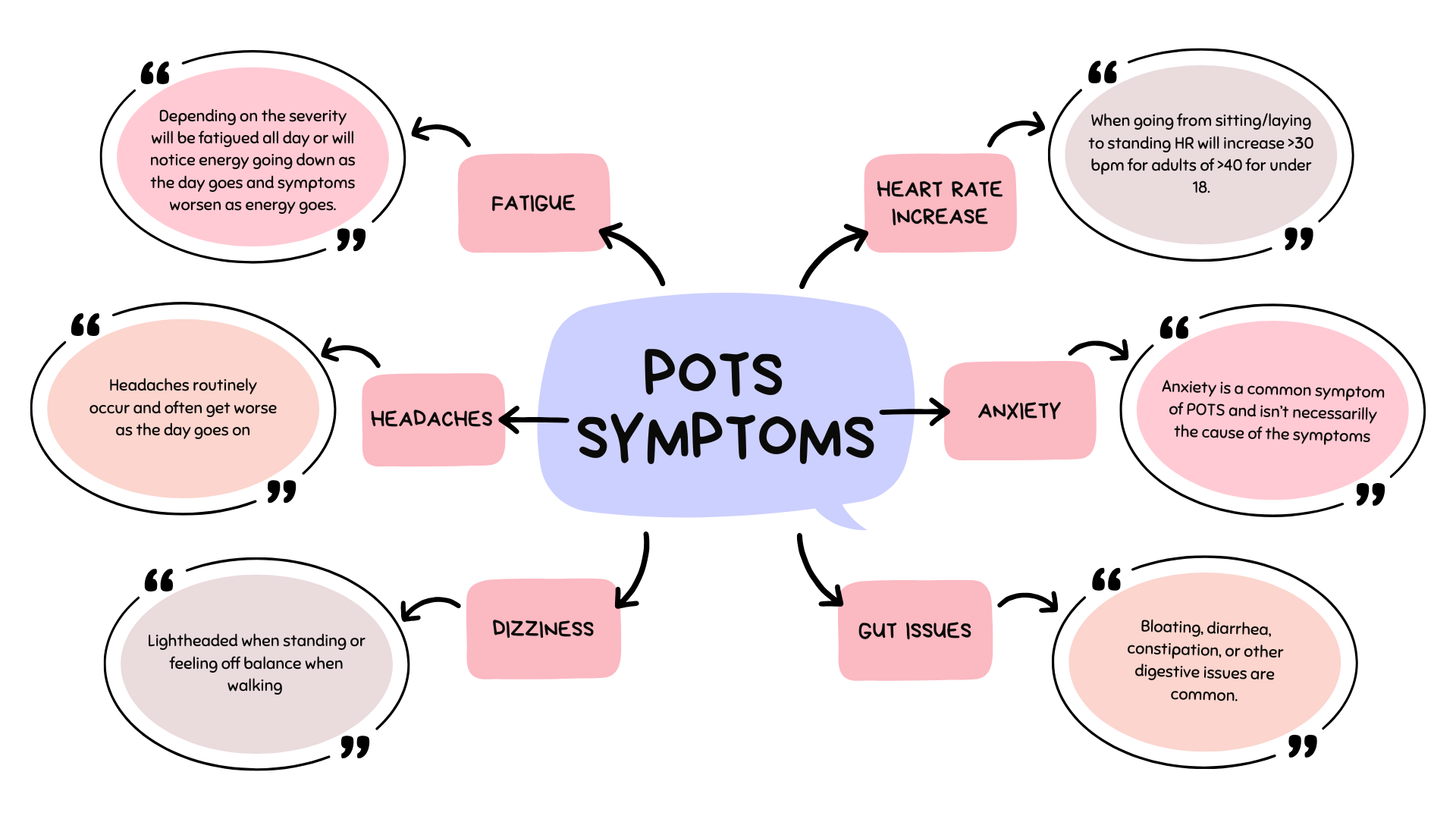
Symptoms of POTS: More Than Just Dizziness
POTS affects multiple body systems, making it difficult to diagnose and manage. Common symptoms include:
- Cardiovascular: Palpitations, fainting, feeling lightheaded, Raynaud’s syndrome (cold, discolored hands and feet)
- Neurological: Brain fog, headaches, dizziness, blurry vision, vertigo, ADHD-like symptoms, anxiety
- Gastrointestinal: Nausea, bloating, constipation, diarrhea, irritable bowel syndrome (IBS)
- Musculoskeletal: Weakness, joint pain, hypermobility, muscle fatigue
- Endocrine: Menstrual cycle irregularities, extreme fatigue, heat intolerance
Many POTS patients find themselves visiting multiple specialists—cardiologists, neurologists, endocrinologists—who only focus on one system. The issue? POTS impacts multiple systems at once. The symptoms above may be associated with the system above, but this is not the underlying reason for the array of symptoms that individuals have. Without a whole-body approach, treatment often falls short, and many are left frustrated.
Why Standard Medical Approaches Fall Short
Most POTS patients are given five main recommendations:
- Increase salt intake
- Wear compression stockings
- Take beta-blockers (like propranolol) to lower heart rate
- If there is a blood pressure drop, which, as we noted this wouldn’t be true POTS, then individuals are given a medication to increase blood pressure.
- Cardiology and neurology often try to work together to send the individual to do physical therapy with a focus on building back up strength and endurance.
While these can help some symptoms, they fail to address the root cause. Many patients feel frustrated when medications like propranolol leave them with brain fog and fatigue, but don’t actually fix what’s causing their POTS in the first place.
Physical therapy, in our experience, often makes these individuals worse as it’s not done at the right time. It’s not as simple as just building up physical endurance; you must identify what is driving the POTS to begin with. After that is treated, then physical therapy or simply going to a gym and working up can go well.
A Smarter Approach to Treating POTS
To understand what to look for in treatment, it’s important to understand that even though it’s often treated as a cardiovascular condition, it’s not for many. It is a neurological and immune-based issue that manifests with a variety of symptoms, with the hallmark feature being heart rate.
To truly improve, you need a comprehensive plan that evaluates:
- Neurological function – Brain imbalances can lead to autonomic dysfunction. Testing eye movements and balance can provide crucial insights into nervous system health.
- Immune system health – Autoimmune issues and chronic inflammation are major drivers of POTS.
- Gut health – IBS and leaky gut can worsen POTS symptoms due to their connection with the nervous and immune systems.
- Mast cell activation & histamine response – Many POTS patients also experience extreme reactions to foods, environmental triggers, and stress.
- Hormonal balance – Menstrual cycles, adrenal dysfunction, and thyroid disorders all influence POTS symptoms.
We will briefly discuss how to evaluate the nervous and immune system in POTS and dysautonomia.
Many people will naturally think they need an MRI or a CT scan due to the headaches, dizziness, and nausea. They are routinely disappointed if they do get one, as this does not provide any information for someone with POTS and chronic fatigue. It should be done if there is a worry of something like a tumor or a brain bleed. It is essential to look at nervous system function.
The eyes are known as the windows into the health of the brain. A comprehensive eye movement assessment should be done using computerized technology known as videooculography. This allows for the highest level of evaluation and is very educational, as it allows you to see where you did well and did not. Components of an eye movement examination should include: vergence, fixation, pursuits, saccades, and optokinetics.
The other side of the neurological evaluation is balance. Balance testing is routinely off with many POTS patients. What we’ve found is that if it’s only balance, then it’s not necessarily something that is treated. If both eye movements and balance are off, then neurological rehab does really well. You may be wondering why it’s not necessarily appropriate to treat poor balance. As you’ve experienced, you notice fatigue, weakness, and an inability to be on your feet too long. When balance is off, it could be due to neurological dysfunction or simply related to the fatigue and weakness many have.
The immune system is initially evaluated by looking at triggers that impact symptoms. What happens when you get stressed, sick, have menses, make food choices, or experience sleep changes? Based on this, it gives the provider a good idea of where to start. Beyond this, it is often beneficial to evaluate immune system markers, gut health, and reactions to mycotoxins from molds.
How We Help People with POTS Recover and Feel Better
At Peak Brain and Body, we take a root-cause approach to POTS and chronic fatigue treatment, using advanced neurological testing, brain function assessments, immune system evaluations, and metabolic panels to uncover hidden triggers. This isn’t just another evaluation or brief visit; this is the most in-depth evaluation most of our patients have ever had.
Here’s what makes our approach different:
- We connect the dots between your brain, nervous system, and immune function.
- We perform in-depth testing beyond standard labs to find hidden infections, gut imbalances, or underlying concussions that may be contributing to your symptoms.
- We use targeted therapies like eye movement therapy, balance retraining, cognitive therapy, low-level laser, hyperbaric oxygen therapy, and functional medicine interventions to restore nervous system balance.
Based on your testing, a customized care plan is created. It’s not just about finding out what is wrong, but knowing the order things should be addressed.
The Path to Healing From POTS and Dysautonomia
Healing from POTS isn’t about finding a magic pill—it’s about finding the right roadmap for your unique body. While no two POTS cases are identical, addressing neurological health, immune balance, and gut function can make a world of difference.
If you’re tired of bouncing from doctor to doctor without answers, it’s time for a different approach. You deserve to work with someone who understands the bigger picture and has the tools to help you get your life back.
At the end of the day, knowledge is power. You don’t have to live with POTS controlling your life. With the right approach, individuals routinely find healing is possible even if they’ve been told nothing else can be done.
Next Steps
- Looking for answers? Schedule a consultation with Peak Brain and Body to start uncovering the root cause of your symptoms.