If you’ve been diagnosed with Postural Orthostatic Tachycardia Syndrome (POTS), chances are you’ve spent years bouncing between specialists, wearing compression socks, increasing salt, and trying prescription after prescription. And despite doing “all the right things,” you’re still exhausted. Still dizzy. Still feeling like your body is out of sync.
Then, out of frustration and desperation, you started looking outside the box: chiropractic, supplements, upper cervical, acupuncture, and more; yet you still aren’t getting better.
You’re not alone. You’re not crazy. It’s not just in your head as a mental health disorder, even though you may have depression and anxiety, but who wouldn’t after struggling for years and being misunderstood.
The reason you haven’t gotten better isn’t because POTS is untreatable—it’s because POTS has been fundamentally misunderstood.
You’ve been told it’s a cardiovascular issue, which is why you keep seeing cardiology. But here’s the reality: POTS is not a cardiovascular disorder. The cardiovascular symptoms are manifestations of dysfunction within your autonomic nervous system. That distinction changes everything. And when you start approaching POTS from the lens of neuroplasticity, you open the door to real, lasting recovery.
What Is POTS…Really?
Let’s get the technical stuff out of the way.
- POTS is diagnosed when your heart rate increases by more than 30 beats per minute (or 40 if you’re a teenager) within 10 minutes of standing up, without a significant drop in blood pressure.
- POTS is diagnosed after multiple symptoms and vital sign changes have persisted for at least 3 months.
- POTS is considered an appropriate diagnosis if there isn’t a better explanation for the symptoms and findings.
But let’s go deeper.
POTS lives under the umbrella of dysautonomia—dysfunction of the autonomic nervous system (ANS), which controls involuntary functions like heart rate, blood pressure, digestion, and temperature regulation.
So while your cardiologist may look at POTS as a heart rate problem, and your neurologist may say, “Not my lane,” the truth is: POTS is a nervous system issue that manifests as symptoms in your cardiovascular, respiratory, and gastrointestinal systems.
That’s why treatments like beta blockers, IV fluids, or Midodrine might reduce your heart rate or help you not feel faint, but they don’t fix the underlying issue. They’re managing symptoms, not creating healing.
What we’ve found in helping individuals for over 10 years and looking at the research, it’s clear that POTS is a nervous system issue that is influenced by impaired neurological and immune function.
Why Neuroplasticity Matters in POTS Recovery
Neuroplasticity is your brain’s ability to change, adapt, and form new connections based on the information it receives. And it can go one of two ways:
- Positive neuroplasticity creates new, healthy patterns.
- Negative neuroplasticity reinforces dysfunctional loops that keep your symptoms alive.
When you’re living with POTS, your brain and nervous system have learned to operate in a dysregulated state. You didn’t choose this, but the longer it goes on, the more deeply those patterns get wired in.
This is why surface-level treatments often fail. They don’t address the why. They don’t rewire the brain. And they don’t promote positive neuroplasticity, which is the only way real, long-term healing happens.
Understanding the Brainstem’s Role in POTS
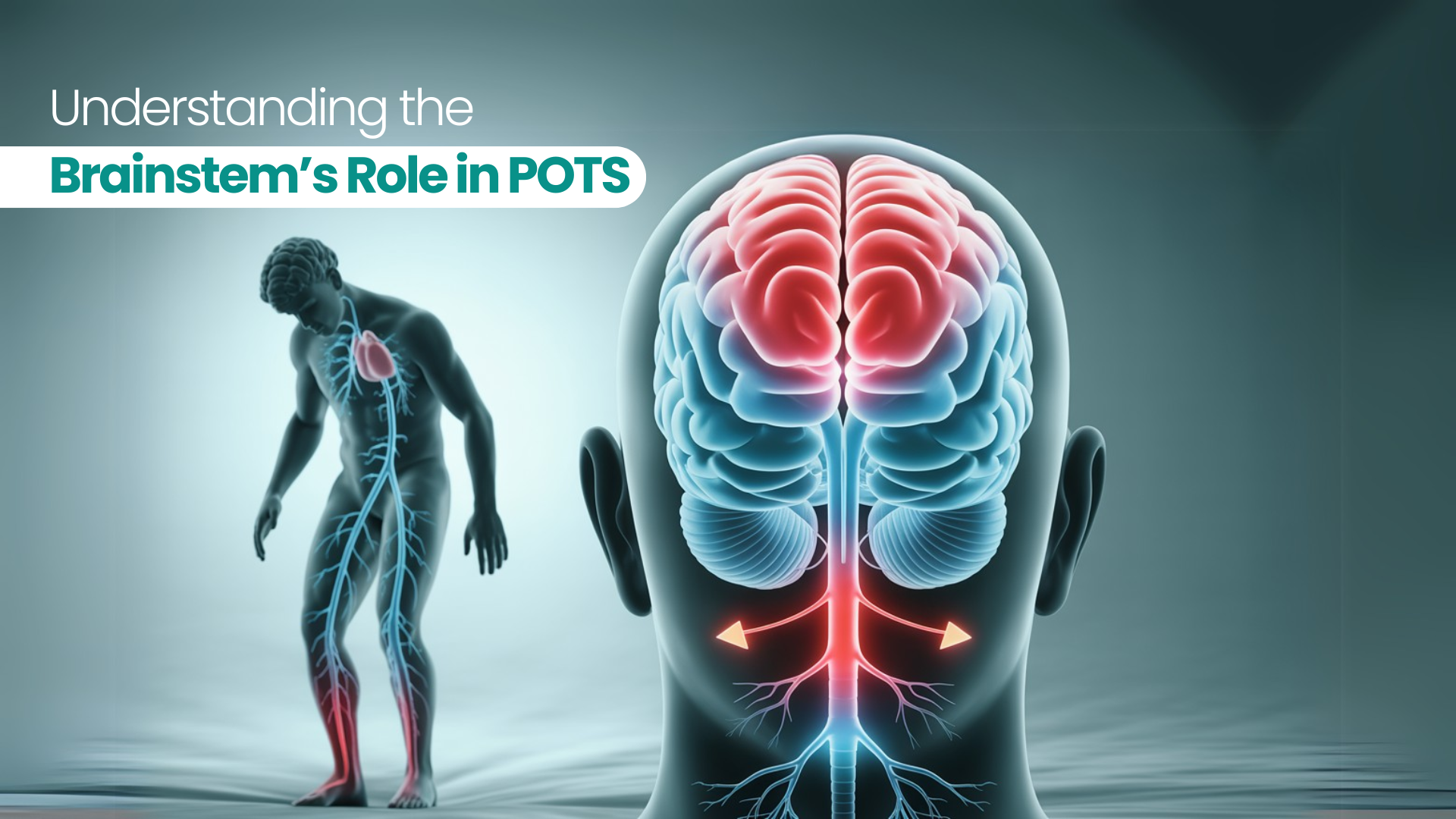
To understand where POTS comes from, we need to look at the brainstem. The brainstem is the lower part of the brain with the lobes of the brain on top of it. When we look at the brainstem, there are 3 parts, but for simplicity, we are going to separate it into 2. The upper half, mesencephalon, is responsible for what’s known as the sympathetic nervous system. The lower half, the pons and medulla, is responsible for what’s known as the parasympathetic nervous system. This area is routinely called the pontomedullary region and is where we are going to focus. It’s the hub for the vagus nerve and integration of a variety of sensory inputs into the brainstem that will impact autonomic function.
The vagus nerve is crucial—it controls heart rate, digestion, blood pressure, and even inflammation. It’s been a hot topic in health circles lately, but we’ve been working with it long before it was trendy.
The vagus nerve is a two-way communication highway. It sends information from the body to the brain, and from the brain back to the body. If that feedback loop is disrupted, your body can’t regulate itself the way it’s supposed to.
For example, when you stand up, baroreceptors (pressure sensors in your arteries) should detect the drop in blood pressure, and this reduces the signals being sent to the brainstem and should result in increased sympathetic outflow to maintain blood pressure.
If this system isn’t working, blood pools in your lower body, your brain gets less oxygen, and you feel faint, dizzy, or like your heart is pounding out of your chest.
Why Treating the Vagus Nerve Alone Isn’t Enough
A lot of people get excited about vagus nerve stimulation, and there’s a place for that. We use tools that target it, and they can help.
But let’s be clear: stimulating the vagus nerve alone is like trying to fix a car by polishing the headlights.
POTS isn’t a “one-nerve” problem. The vagus nerve is just one player in a much larger system. Your brainstem, cortex, cranial nerves, cervical spine, and vestibular system all work together to regulate your autonomic function.
If you’re only targeting one piece of the puzzle, you’re going to keep missing the full picture and won’t get better.
The Vestibular System: The Overlooked Player in POTS
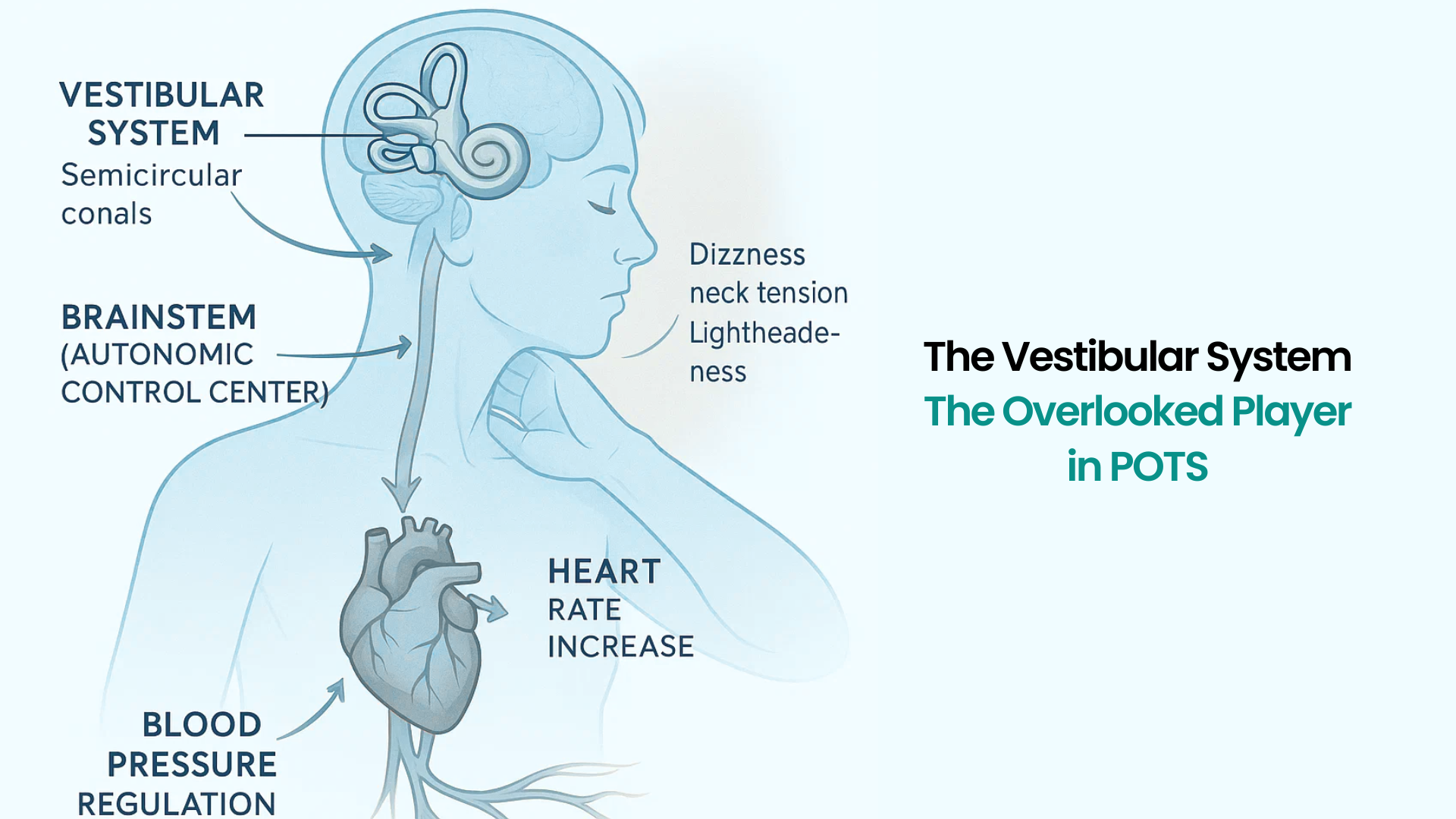
Your vestibular system, which controls balance and spatial orientation, is deeply intertwined with your autonomic function.
When you move your head, bend over, or shift positions, your vestibular system helps regulate blood pressure and heart rate through vestibulo-autonomic reflexes known as the vestibular sympathetic reflex.
If your vestibular system is out of sync, your blood pressure can crash when you move, and your heart rate can spike inappropriately. This is especially true if you have orthostatic hypotension, as impairments in the vestibular sympathetic reflex is the major contributor to this process.
Unfortunately, most with POTS, orthostatic hypotension, or other forms of dysautonomia will never have a vestibular evaluation. When people think of vestibular issues, they often think about issues with the inner ear resulting in vertigo.
In fact, many people with POTS don’t even have classic vertigo, but they still have vestibular dysfunction. That’s why dizziness, lightheadedness, neck pain, and motion sensitivity are so common.
We run computerized vestibular testing and eye movement tracking (video-oculography) on every patient, and over 75% show abnormalities. If your provider isn’t testing this, they’re missing one of the biggest drivers of your symptoms. In our experience, if this isn’t done, then you won’t get better if it was something that should have been treated.
The Cervical Spine, Vision, and Balance: Why It All Matters
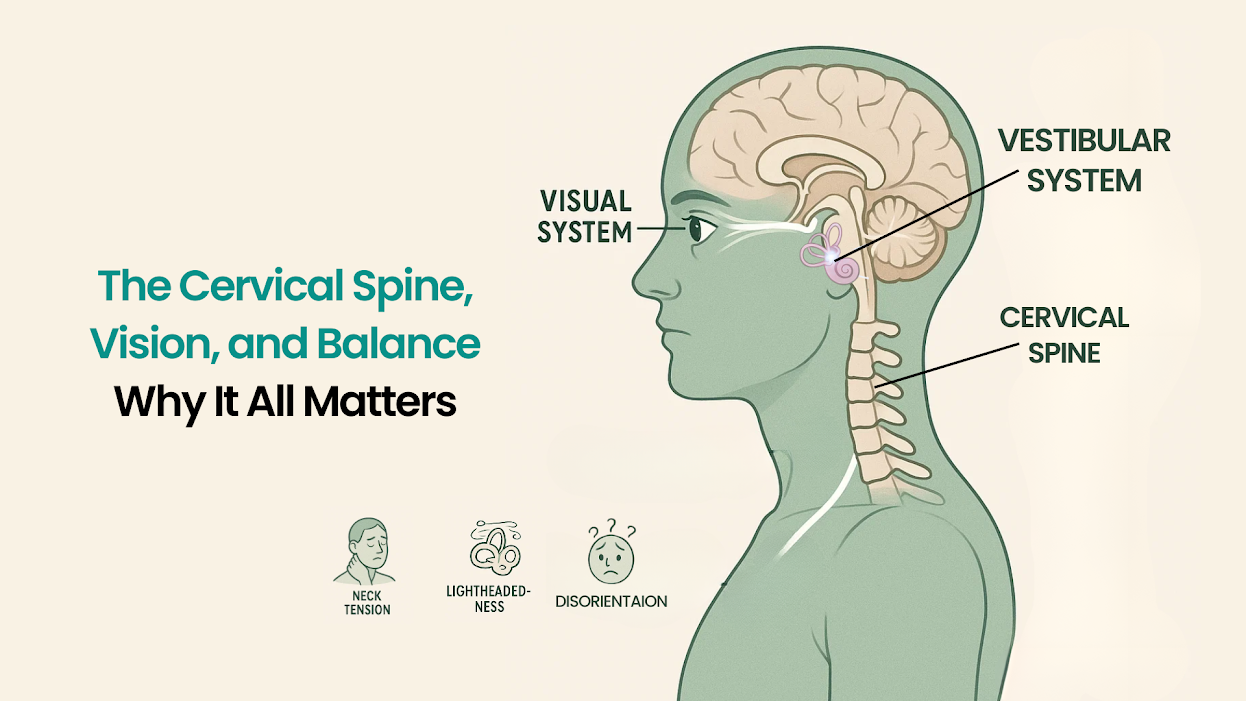
Your neck (cervical spine) contains joints and muscles that feed into your vestibular system. When this information is good, it helps to stabilize the vestibular system, but when it’s bad, it can contribute to issues with the vestibular system. Problems here can mess with your balance, your blood pressure regulation, and your brain’s ability to orient in space.
But again, adjusting the neck alone won’t fix POTS. I’ve been in this field for over a decade. I’m a chiropractor and a nurse practitioner. I’ve seen neck adjustments help, but rarely do they solve the problem. I know you’ve likely heard in groups that some miracle happened with regular chiropractic, upper cervical, or yucca-based approach. Yes, some individuals do get better with it, but it’s not many, and we are about predictable results, which is why stopping with the cervical spine isn’t enough.
That’s because your visual system plays a role too. Your eyes work in tandem with your vestibular system to stabilize your vision and sense of movement. If your eye movements are off, even just slightly, it creates chaos for your brain and nervous system.
If scrolling your phone, driving, or being in crowds makes you feel “off,” that’s your oculomotor system screaming for help.
That’s why we test it. Every patient. Every time.
Immune and Inflammatory Triggers
Now let’s talk about what makes everything worse: inflammation and immune dysfunction.
If you notice your POTS symptoms flare up during:
- Menstrual cycles
- Seasonal allergies
- Illness or infections
- After eating certain foods
…it’s likely because of neuroinflammation. Inflammation disrupts neuroplasticity and puts your nervous system on high alert. It changes how your brain processes signals, making symptoms feel more intense and harder to recover from.
This is where comprehensive lab testing becomes critical.
I’m not talking about basic panels, 3-5 vials, that come back “normal.” I’m talking about in-depth panels that look at gut health, nutrient deficiencies, autoimmune markers, and mitochondrial function.
Because if your body doesn’t have the fuel due to metabolic issues, or the immune system has shifted in the wrong direction, no amount of physical therapy or salt loading will move the needle.
The Mitochondrial and Hormonal Piece

There’s another layer most clinics skip: cellular energy.
Your nervous system runs on ATP—energy made by your mitochondria. If your mitochondria are sluggish (due to infections, toxins, stress, nutrient issues, or hormone imbalances), your brain can’t regulate itself. Did you know your brain uses 25% of the entire bodies energy supply when you are at rest?
Now, what happens when you have an unhealthy nervous system that is burning fuel inefficiently? Everything only gets worse. There are also a variety of factors that contribute to the energy capacity of the brain beyond neurological connections.
You may also have:
- Thyroid issues (especially missed subclinical hypothyroidism)
- Anemia
- Adrenal dysregulation
- Sex hormone imbalances
All of these affect how your brain functions—and whether your nervous system can rewire itself properly.
So… What Actually Works?
Here’s the framework we follow at Peak Brain and Body:
- Comprehensive Evaluation
We run tests that others skip:
- Computerized vestibular and balance testing
- Video eye movement analysis
- In-depth neurological examination
- Expanded lab panels to identify immune and metabolic patterns
- Multisystem Treatment Plan
We don’t throw darts in the dark. With the amount of data we gathered, we confidently tailor your treatment to what your body is telling us. That might include:
- Neuroplasticity exercises targeting visual, vestibular, and motor systems
- Brainstem and cerebellar retraining
- Vagus nerve modulation
- Cervical spine rehabilitation (if appropriate)
- Mitochondrial and hormone support
- Immune modulation and gut healing
- Pattern-Based Progress
We don’t chase symptoms—we follow patterns. The more patterns we identify, the more accurately we can target treatment. It’s like studying the whole textbook before the test, not just one chapter.
This is where patience has to come in, just because we find something, it doesn’t mean it’s the first thing we have to address. If we address the wrong thing at the wrong time, you won’t get the results you want. We’ll guide you based on the patterns and testing to identify what should be addressed when.
Why You’re Still Stuck (And How to Change That)
If you’ve tried supplements, hyperbaric therapy, IVs, chiropractic, or functional medicine, but never got real traction, it’s not because you’re broken.
It’s because your care has been fragmented.
You’ve done bits and pieces. But this is like trying to bake a cake by only using flour. You need all the ingredients, and you need them in the right order.
When we bring all the systems together—neurology, cardiology, immunology, endocrinology, and gut health—we see people get their lives back.
Most of our POTS patients improve by 70-80% or more. The time to achieve those results is dependent on the underlying reasons why POTS is an issue for you. Some need additional support beyond the initial plan. But when you work through this framework systematically, the body starts to heal.
Final Thoughts: You’re Not Crazy. You’re Just Misunderstood.
If you’re reading this and thinking, “Why hasn’t anyone explained this to me before?”—that’s exactly why I created this blog.
Most providers weren’t trained to think this way. But this is the future of care for complex neurological conditions like POTS.
At Peak Brain and Body, we see patients from all over the country—people who’ve seen 10+ doctors and still didn’t have answers. But when you finally look at the full picture, things start to make sense.