If you’re reading this, there’s a good chance you’re still living with the effects of a concussion—whether it happened recently or years ago. Maybe you’ve been struggling with concussion symptoms like brain fog, fatigue in concussion, dizziness, concussion headache, or mood changes. Maybe you’ve tried physical therapy, chiropractic, medications, or supplements, and yet… something still feels off.
You’re not alone—and it’s not in your head despite the likelihood you’ve been told multiple times it’s from anxiety, depression, or that a concussion can’t impact you for that long. Concussions are the most common type of traumatic brain injury and are often classified as mild traumatic brain injury.
In this post, I’m going to walk you through everything you need to know about post concussion syndrome treatment in Tampa—from how concussions are (often wrongly) diagnosed, to the most common concussion myths, and most importantly, what proper post concussion treatment should actually look like.
Because what most people are getting isn’t sufficient? It’s not the full picture. And that’s why Peak Brain and Body is a leader in post concussion recovery and post concussion clinic care in Tampa and beyond.
This is the information I wish someone had given my wife 15 years before we finally discovered the root cause of her daily symptoms. She shouldn’t have had to suffer with daily headaches amongst many other symptoms.
There is a video version here: https://youtube.com/live/zdA0fYzWMw4
Why I Care So Much About Concussions (And Why You Should Too)
This is personal for me.
My wife had three concussions in her younger years. For over a decade, she battled with brain fog, fatigue in concussion, dizziness, and mood swings. She went to a couple doctors and was told it was just hormones, puberty, or stress. Even if she brought it up to her parents, the reply was “you’ve already been to the doctor.” No one put the pieces together. No one ever said, “Hey—this might be from a brain injury.”
That changed when I was working in a brain injury clinic. She realized that the concussion symptoms that individuals were having resolved on a daily basis were part of her everyday life. They were so common that she didn’t even mention them, because weren’t those symptoms that most people had? We finally did the right evaluations, uncovered what was missed, and began treatment that actually addressed her brain function. It was the beginning of her healing—and it changed the trajectory of my career.
Since then, I’ve dedicated my life to helping people who’ve been struggling silently for far too long.
People like you.
People who know something’s wrong but can’t get clear answers or real solutions. People who’ve been dismissed or told “you’re fine” based on a 5-minute exam or a normal MRI. People who’ve been told to “just wait it out” or “it’s all anxiety.” People who’ve tried functional medicine and been told maybe it was their thyroid, hormones, or gut health when in reality it was an unresolved concussion. In my experience, nearly 90% of those still struggling with concussion symptoms have no clue that is the driving factor for the symptoms they have.
I see you—and I want you to know: there’s hope. And there’s help.
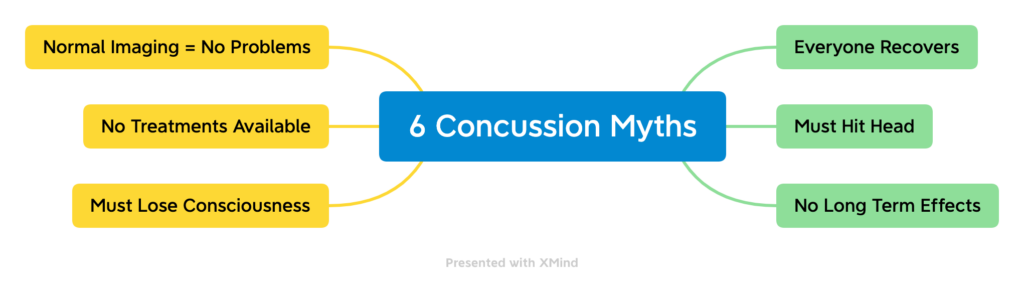
The Most Common Concussion Myths That Keep People From Healing
Let’s start with some hard truths—because these concussion myths are harming people every single day. You’ve been told these from family, friends, co-workers, and even worse other medical providers:
“You didn’t lose consciousness, so it can’t be a concussion.”
False. About 90% of concussions don’t involve loss of consciousness. That’s not a requirement.
“You didn’t hit your head.”
Also false. A whiplash injury—like in a car accident or fall—is more than enough to cause a concussion. You don’t need a visible bump or bruise on your head. In our experience, concussions are the most undiagnosed and untreated injuries that occur in a car accident.
“Your imaging came back normal.”
This one makes my blood boil. A normal CT or MRI just means there’s no bleed or fracture. It says nothing about brain function or about a possible concussion. Most concussions won’t show up on those scans as they aren’t made to detect it. That doesn’t mean you’re okay, even if a provider says your imaging looks good and you are fine. This isn’t true and don’t fall for it.
“You just need to rest and wait it out.”
Maybe that made sense 20 years ago based upon our limited understanding of the brain. But if you’re still being told to sit in a dark room and “wait it out,” you’re not being given current, science-backed guidance. In fact, that kind of advice has been shown to delay your recovery.
“You’re just anxious or depressed.”
Yes, concussions can affect mood—but brushing off your brain-based symptoms as “mental health” issues without evaluating your brain is a huge disservice. We know that it’s very common to develop depression or anxiety after a concussion. We also know that pre-existing depression prolongs concussion recovery and tends to worsen symptoms. That doesn’t mean it is all from depression, but the way these issues interact with concussion recovery.
Post-Concussion Syndrome Symptoms
Maybe you’ve had a concussion and were told you’d bounce back in a few weeks—but here you are, months or years later, still not feeling like yourself.
Here are some of the concussion symptoms we commonly see in people with undiagnosed or untreated post concussion syndrome:
-
Brain fog that makes it hard to think clearly or find words
-
Fatigue in concussion cases that worsens throughout the day and doesn’t improve with rest
-
Concussion headache or pressure in your head
-
Concussion neck pain or stiffness
-
Difficulty focusing or remembering things
-
Light and sound sensitivity
-
Dizziness, motion sensitivity, or nausea
-
Irritability, anxiety, or mood swings
-
Sleep issues—either insomnia or waking up unrefreshed
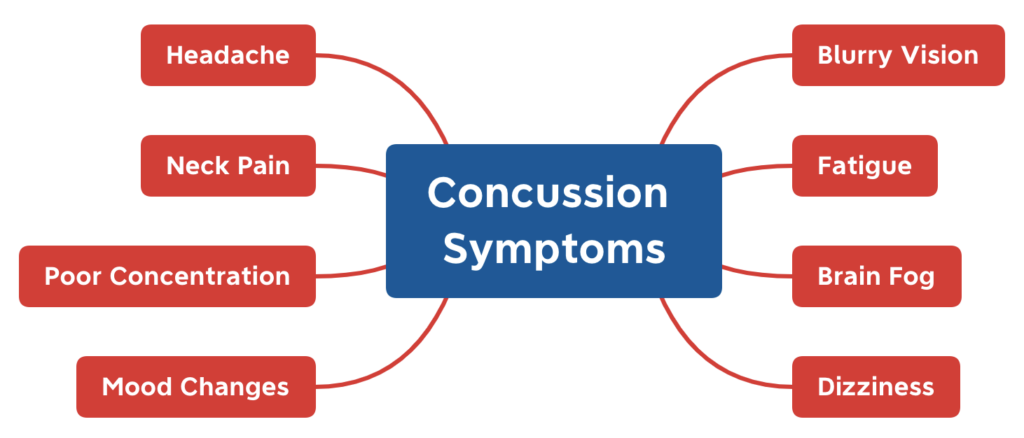
If two or more of these symptoms got worse after your injury—or even if they were already present but intensified—your brain may be struggling to function normally. And you deserve to know why.
How Is a Concussion Diagnosed
Here’s how we determine whether your concussion symptoms are linked to a past injury:
1. A Clear Mechanism of Injury of Concussion
This could be a car accident, fall, sports collision, or any event involving a blow to the head or body that jolts the brain.
2. Clinical Signs of Concussion
Clinical signs would be findings that occur at the time of the concussion. This includes vomiting, loss of consciousness, confusion, and gross motor instability. You do not need to have these to be diagnosed if you have parts 1, 3 and 4.
3. New or Worsened Symptoms of Concussion
According to clinical guidelines, having two or more new or aggravated symptoms is enough to raise a red flag.
4. Objective Clinical Findings of Concussion
This includes eye movement testing, computerized balance assessments, and vestibular evaluations. (More on that in a second.)
5. No Better Explanation
If your symptoms don’t line up with another condition, and testing reveals brain dysfunction, a concussion diagnosis makes clinical sense—even without imaging abnormalities.
Here is a graphic from the American Congress of Physical Medicine and Rehabilitation for diagnostic criteria for MTBI.
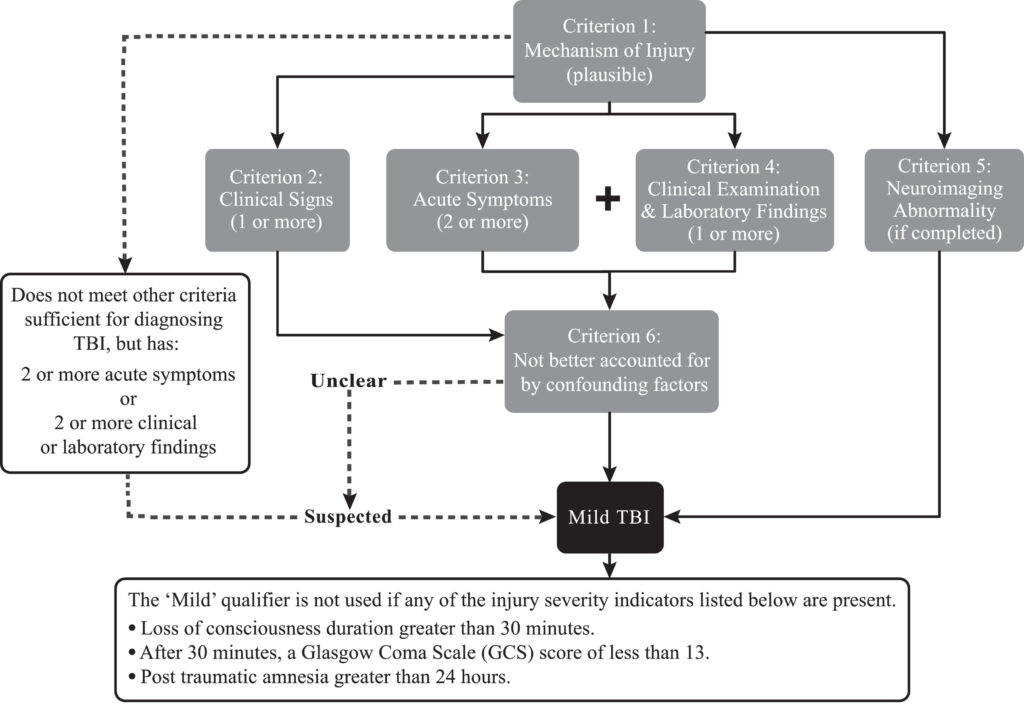
The American Congress of Rehabilitation Medicine Diagnostic Criteria for Mild Traumatic Brain Injury
Silverberg, Noah D. et al.
Archives of Physical Medicine and Rehabilitation, Volume 104, Issue 8, 1343 – 1355
Why Most People Aren’t Diagnosed Properly For Concussion
Too often, people are told, “Your scans are normal. You’re fine.” They might get a quick check of reflexes and be sent on their way. It’s unfortunate that this happens, but most providers receive little to no training on concussions.
Here’s what’s missing, objective testing:
Computerized Balance Testing
This shows how well your brain integrates signals from your eyes, vestibular system, and body. The platform measures how much you move on a firm and perturbed surface with eyes open and closed. Beyond this, evaluating tandem stance and one legged stance is also important.
Eye Movement Testing (Video Oculography)
We use specialized goggles to record your eye movements. Why? Because your eye movements are directly connected to brain function. It is important to measure gaze fixation, pursuits, saccades, anti-saccades, optokinetics, and spontaneous nystagmus. If you can’t smoothly follow a target, your brain isn’t processing information correctly and this will routinely cause a variety of symptoms.
QEEG Brain Mapping
This measures your brainwave activity. While not diagnostic on its own, it’s a powerful way to measure progress and see how your brain is functioning. In the future, this testing will likely be more important as research will be able to correlate certain brainwave patterns with concussions.
Why Most Treatments Fail (And What You Actually Need)
Many try one therapy at a time—vision therapy, vestibular rehab, neurofeedback—yet still don’t recover. That’s because concussions affect multiple systems.
You need an integrated plan addressing:
-
Neurological dysfunction
-
Brain energy production
-
Vestibular & visual processing (concussion Oculomotor therapy, concussion Vestibular therapy)
-
Inflammatory & immune factors
-
Pre-existing health
Think of it like trying to play your favorite song—but each instrument is playing solo. You need them all working together in harmony as that is the only way you get the results you want.
Post-Concussion Syndrome Treatment in Tampa at Peak Brain and Body
At our clinic, we go beyond checklists and guesswork. Every treatment plan is custom-built based on detailed testing. And instead of treating one system in isolation, we stack therapies together in a sequence that makes sense for your brain.
Our Treatment Toolbox Includes:
- Oculomotor therapy is based on improving the brain’s ability to perform a variety of functions.
- Vestibular therapy to integrate the function of vestibular, visual, and cervical spine.
- Postural and neck retraining
- Photobiomodulation (laser therapy) to reduce inflammation and support cellular energy
- Brain-based cognitive training and hand-eye coordination drills
- Targeted supplementation and peptide therapy
- Functional medicine to address root issues like gut health, hormones, autoimmunity, or mold exposure
We do all of this in a way that’s dynamic—just like your brain. And it works.
Real Recovery Is Possible
If you’ve been told there’s nothing else you can do, I want to tell you this: That’s not true.
I’ve seen people who’ve been struggling for 5, 10, even 15 years start to recover—because someone finally asked the right questions and ran the right tests.
I’ve seen people go from canceling plans and calling off work… to being present with their families again. Getting their careers back. Enjoying life again.
And the best part? Most people don’t need lifetime care. They need the right care at the right time—tailored to their brain. The brain can change fast when it’s provided the right information and supported.
You’re Not Broken. You’re Just Misunderstood.
If you’ve been told your symptoms are all in your head, or that you should have recovered by now—let me say this loud and clear:
You’re not crazy. You’re not lazy. And you’re not broken.
You’re dealing with a brain that hasn’t fully recovered. And once we understand where the disconnects are—we can start fixing them.
It doesn’t matter what you’ve tried in the past, our clinic is full of individuals who tried numerous other therapies before they finally came in and found answers and solutions.
Ready to Take the Next Step?
If you’re in the Tampa area or are willing to fly in and you’re ready for real answers—and real progress—we’re here for you.
Peak Brain and Body, located in Wesley Chapel, FL, offers the most advanced post-concussion syndrome treatment in the Tampa metro area. It’s led by Dr. Zimmerman who is a best selling author and the only dual-licensed nurse practitioner and chiropractor integrating advanced neurological diagnostics, functional neurology, functional medicine, and peptide therapy in the state of Florida and one of a few in the entire United States.
Click below to schedule your comprehensive brain health evaluation and take the first step toward feeling like you again.
Can post-concussion syndrome symptoms come and go over time?
Yes. People with post-concussion syndrome symptoms timeline often notice that dizziness, headaches, or trouble concentrating may improve for a while and then return, especially if they overexert physically or mentally. Tracking your symptoms over weeks and months can help guide recovery strategies.
Is vestibular rehab only for severe post-concussion dizziness?
No. Vestibular rehab for post concussion dizziness can help even in mild cases. The therapy aims to retrain your brain and inner ear to work together, reducing imbalance and improving stability, regardless of symptom severity.
How does oculomotor therapy help after a concussion?
Oculomotor therapy after concussion focuses on restoring normal eye movement control, which is often disrupted. This can help reduce blurred vision, improve reading ability, and ease headaches linked to visual strain.
What role does neurotherapy play in concussion recovery?
Neurotherapy for concussion recovery uses brainwave training to support cognitive function, mood regulation, and energy levels. It can be combined with physical therapy for a more comprehensive healing plan.
Why is sleep hygiene important in concussion recovery?
Good sleep hygiene concussion recovery tips—such as setting a regular sleep schedule, limiting screen time before bed, and creating a calm environment—are critical because the brain heals most effectively during deep rest.