At Peak Brain and Body, we see the impact of concussions every single day. And yet, despite all the headlines, medical advancements, and increasing awareness, too many children and teenagers are still suffering in silence—misdiagnosed, misunderstood, or completely missed altogether.
This blog is for the parents who feel something isn’t right. This isn’t just your children, but it may explain some of the issues you’ve had since you were a teen that you didn’t know were linked. For the young adults who can’t explain why they feel different. For the healthcare professionals who want to understand what the research says.
We’re going deep into the connection between concussions and mental health, specifically in children and adolescents. And we’re doing it from an evidence-based perspective, so we can shine a light on what’s going wrong… and what can be done about it.
When you understand the evidence, you’ll understand what is truly happening and know that it’s much more than a mental health issue — especially when considering the mental health after concussion.
Concussions Are Not Just a Sports Problem
Every year, millions of concussions go undiagnosed.
Yes, we hear about sports-related concussions—football, soccer, hockey, and gymnastics. But guess what? More concussions occur from car accidents and slip-and-falls than from sports. Yet, if you don’t play sports, you might never get evaluated. That’s a massive issue. Even if you do play sports, many are never evaluated, or they are brushed away because the athlete only cares about returning to the game.
- Parents often miss it.
- Coaches brush it off.
- Even providers cling to outdated thinking from their own childhood experiences and are not up to date or even set up to properly evaluate concussions.
And that bias? It’s ruining lives for not just weeks, but decades. Often, families are unsure how to tell if my child has a concussion, which leads to missed diagnoses.
Lingering Symptoms Aren’t Rare—They’re the Norm
If you think everyone just “bounces back” from a concussion, the research says otherwise:
- 70% still suffer from headaches post-concussion
- 70% report difficulty concentrating
- Over 50% still feel fatigued
- Brain fog, head pressure, mood swings, light sensitivity, memory issues—these are not rare symptoms
- Nearly 50% of individuals still deal with significant symptoms 6–12 months later
Many of these persistent issues point to the long-term effects of concussion, which can affect multiple areas of life — school, work, relationships, and emotional health.
The Link Between Concussions and Mental Health
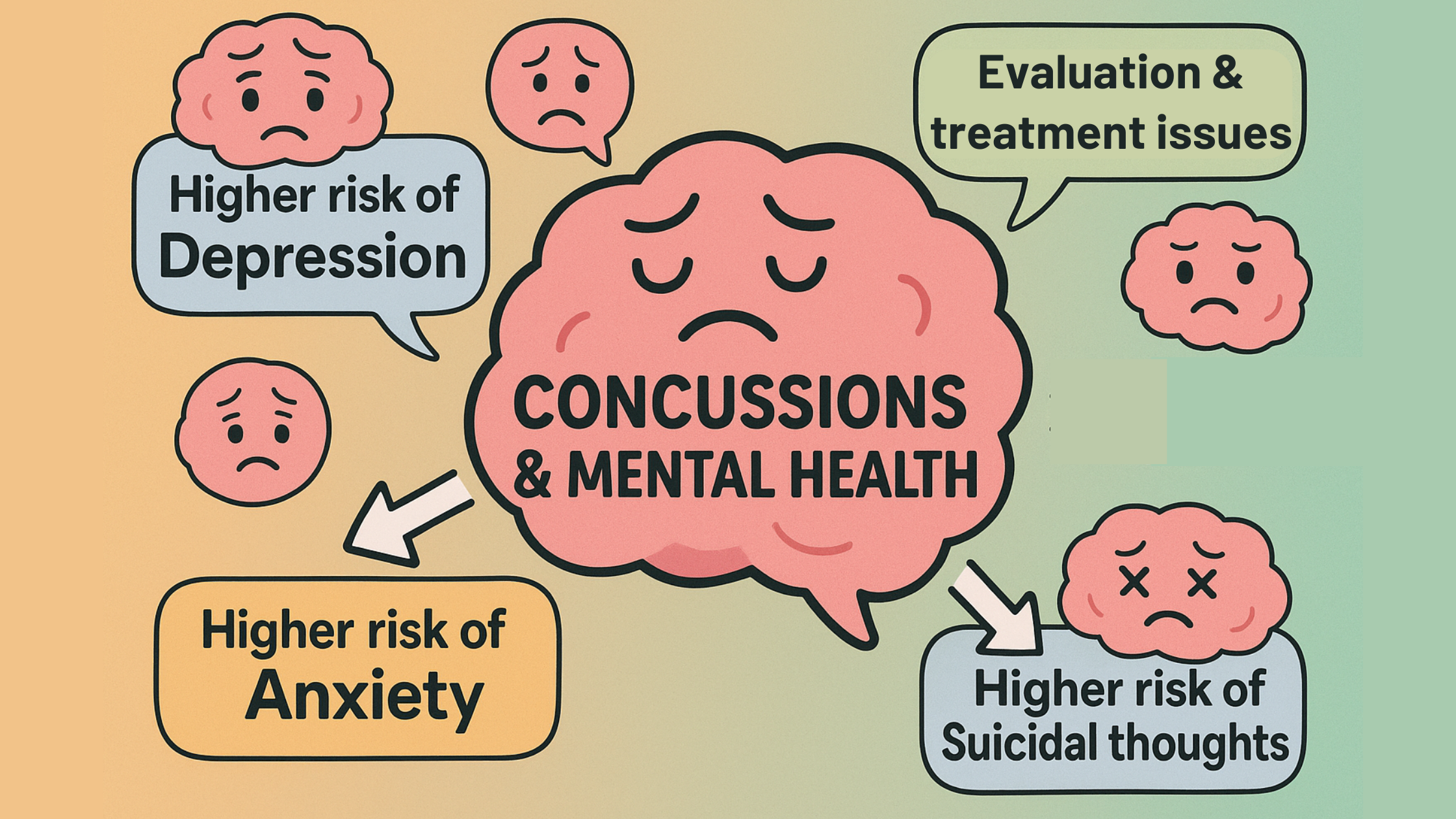
Concussions can significantly affect mental health, increasing the risk of anxiety
Research continues to show staggering associations between concussions and mental health conditions:
- 3.3x greater risk for depression diagnosis in adolescents with concussion history
- 2x higher risk of suicide ideation and attempts after mild TBI
- Increased anxiety, social withdrawal, loneliness, and even substance abuse
- Children discharged from ERs with a head injury were misdiagnosed up to 25% of the time—sometimes labeled with ADHD, sleep disorders, or behavioral issues instead of properly identifying the concussion
In fact, many parents report later, “my child was misdiagnosed with ADHD,” only to realize the real issue stemmed from a brain injury. Some of these cases also develop into concussion-related depression that isn’t caught in time.
And here’s the kicker: many of these kids were never evaluated appropriately. They didn’t get a full neurological workup. For those who were diagnosed, they routinely aren’t even educated on the significance of their injury.
Misdiagnosis = Mistreatment = Prolonged Suffering
Imagine this scenario:
Your child has trouble focusing after a bike crash. The doctor prescribes Ritalin because the teachers and you have noticed a difference in their school performance.
But they don’t have ADHD. They have a concussion that hasn’t healed and is leading to brain dysfunction, which manifests as easily distractible, zoning out, and behavior changes.
Now, their lives have become harder. The medication doesn’t help. They’re still foggy, moody, withdrawn. And because the real issue wasn’t treated, they continue to suffer needlessly for months or years.
That’s not just poor care. That’s dangerous as it ruins what those individuals should have become.
It’s Not “Just Puberty.” It Might Be a Concussion.
Another thing that often gets blamed for these symptoms, is puberty. A teenager who becomes more withdrawn, anxious, irritable, or tired isn’t just “being a teenager.”
Too many families are told their kid is “just hormonal.” But when you dig into their history you discover falling off a bike, a rough tackle in soccer, a fender-bender. They had a clear mechanism of injury that was never evaluated.
If you treat them for anxiety but ignore the neurological root, they don’t get better. They just become another statistic of untreated concussion symptoms in children.
Brain Injury Changes the Brain—Literally
What happens to the brain after a concussion?
Advanced imaging and research studies are showing:
- Changes in brain connectivity—especially in areas tied to attention, emotion, and executive function
- Increased connectivity in the default mode network (often linked with depression and anxiety)
- Persistent alterations in cerebral blood flow and white matter integrity that persists a year after the injury, even in the absence of symptoms
This neurological dysregulation is a major driver of mental health after concussion, contributing to lasting emotional and cognitive issues.
But here’s the problem: most of this testing isn’t available in routine clinical care. That’s why it’s so important that your provider is highly trained and uses the best tools available to evaluate function, not just symptoms.
Most Concussion Evaluations Are Incomplete
Let’s get this straight. A proper concussion evaluation is not just asking, “Did you hit your head?” and “Do you have a headache?”
At Peak Brain and Body, we follow the American Congress of Physical Medicine and Rehabilitation’s criteria, which includes:
- A clear mechanism of injury (car accident, whiplash, sports hit, etc.)
- At least two or more symptoms within 48 hours
- Clinical examination findings such as:
- Cognitive impairment
- Balance impairment
- Oculomotor impairment (eye movements and visual tracking)
Unfortunately, many providers rely only on cognitive testing. But cognitive testing alone is not enough. A full workup should include:
- Computerized balance testing
- Video oculography (eye movement and visual processing testing)
- Neurological examination
- Metabolic and laboratory evaluations
Because here’s the truth: if you don’t ask the right questions, you don’t get the right diagnosis, which means you certainly don’t get the right treatment.
What About Imaging?
CTs and MRIs are typically normal in concussion cases. We understand how frustrating it is when you are told that your imaging is normal. Just because imaging is normal, doesn’t mean that everything is normal. It means that it’s not the best way to assess a concussion. The testing is as we discussed above. If there was imaging that could be done, it’d be functional imaging.
Functional imaging like SPECT or advanced MRI sequences can show changes, but they’re rarely done outside research settings as it’s very expensive. That’s why we use objective clinical testing to measure recovery and guide care, not just rely on standard imaging.
Why Standard Treatments Fall Short
A visual comparison between medication and holistic approaches to mental wellness
The journey that most individuals go through following a concussion diagnosis should sound very familiar.
You will see a primary care provider who will tell them this is something that you should recover from in a couple of weeks. If after a couple of weeks you are still struggling, you will be sent to a neurologist to see if there is anything else that should have been addressed. If you have severe enough symptoms, specifically migraines, then a neurologist will prescribe you medication for it. But if you have mental health symptoms, you will then be sent to a psychiatrist, where you’ll be recommended additional medications.
Because you’ve been going to your primary care provider and you are complaining of neck pain, headaches, and maybe some dizziness, they will send you to physical therapy. Most physical therapy places use a very generic treatment program that is going to help some, but because it’s not tailored to your needs, you will not get the results you want. This is going to lead to frustration, and you are going to go to the internet (via social media and web browsing) out of desperation and pick a lot of things that may sound good.
Many people come to us after trying hyperbaric oxygen, neurofeedback, chiropractic, acupuncture, or IV therapy.
Let me be clear: NONE of these treatments fix every concussion.
They may be helpful as part of a plan—but if someone tells you their one tool is the magic bullet for concussions, you need to run the other direction.
Recovery requires stacking therapies strategically. At Peak Brain and Body, we tailor combinations like:
- Vestibular rehabilitation
- Eye movement therapy
- Hand-eye coordination exercises
- Cognitive retraining
- Laser therapy for brain injury
- Mild hyperbaric oxygen
- Nutritional and peptide support
- Lifestyle and metabolic optimization
This integrated approach is where people get results—especially when they’ve failed elsewhere. We also follow the 6 stages of concussion recovery to ensure no step is missed.
The Brain Doesn’t Heal in Isolation
Don’t forget: brain health is body health.
If someone has low iron, blood sugar issues, autoimmunity, poor thyroid function, hormone imbalances, chronic infections, or extreme stress—it’s going to interfere with brain healing.
That’s why every new patient at Peak Brain and Body gets an in-depth history and lab workup. Because if we don’t know what’s sabotaging recovery, we can’t fix it.
We are routinely told from individuals that their labs are normal, but with more advanced testing we often find pivotal information that impacts recovery.
Final Thoughts: Rethink Mental Health and Concussions
Mental health struggles, especially in children and teens, are often not what they seem. Depression, anxiety, behavioral issues… they may be symptoms of an unhealed brain injury.
At Peak Brain and Body, we don’t chase symptoms. We investigate root causes.
If your child, your teen, or even you have unexplained mental health challenges and a remote history of a possible head injury, even without a formal concussion diagnosis, you deserve a proper evaluation.
Because until we stop blaming mental health as a standalone issue and start asking what’s driving it, people will continue to suffer.
It’s time to do better.
If you’re ready to uncover the real reason behind lingering symptoms, or help your child finally feel like themselves again, reach out. We’re here to help.
______________________________________________________________________________________
Located in Wesley Chapel, FL, Peak Brain and Body is a destination for individuals seeking world-class care for concussions, brain fog, POTS, and complex neurological conditions.
Patients travel from across the U.S. for our cutting-edge diagnostics and integrated recovery programs.
Call us today or schedule your Health Strategy Session to get started.