Functional Neurology Tampa: The Future of Brain Health and Rehabilitation
Dr Zimmerman
on
March 8, 2025
In the ever-evolving landscape of healthcare, functional medicine has taken center stage in offering a more personalized, in-depth approach to wellness. But within this movement, one of the most transformative and underrecognized fields is Functional Neurology—a groundbreaking approach that holds the key to unlocking solutions for a vast array of neurological conditions and symptoms. You will learn there are many common symptoms that individuals don’t routinely associate with brain health but they actually are.
At Peak Brain and Body in Wesley Chapel, near Tampa Bay, Dr. Spencer Zimmerman stands at the forefront of this revolution. As one of the nation’s most sought-after practitioners who combines functional neurology chiropractic care with functional medicine, his expertise extends far beyond state lines—patients from across the country and even internationally travel to see him, seeking answers that conventional neurology has failed to provide. If you’ve ever searched for a “functional neurology center” or wondered about “functional neurology near me,” Peak Brain and Body is a destination that offers advanced answers and results.
Here is the video version: click here
What Is Functional Neurology?
Functional Neurology is an advanced, non-pharmaceutical approach to diagnosing and treating neurological dysfunctions. Unlike traditional neurology, which largely relies on MRIs, CT scans, and pathology-based diagnostics, functional neurology delves into how the brain is functioning rather than just identifying structural damage. By assessing eye movements, balance, coordination, cognitive function, and movement patterns, functional neurology evaluates the intricate connections within the brain to pinpoint dysfunction and develop targeted rehabilitation strategies.
Functional neurology is built on the foundation of neuroplasticity—the brain’s ability to adapt, reorganize, and heal itself based on stimulation. By leveraging precise rehabilitation techniques, functional neurology helps retrain the brain, optimize neural pathways, and restore lost function.
Who Can Functional Neurology Help?
Dr. Zimmerman and his team at Peak Brain and Body have treated thousands of patients suffering from a wide range of complex neurological conditions, including:
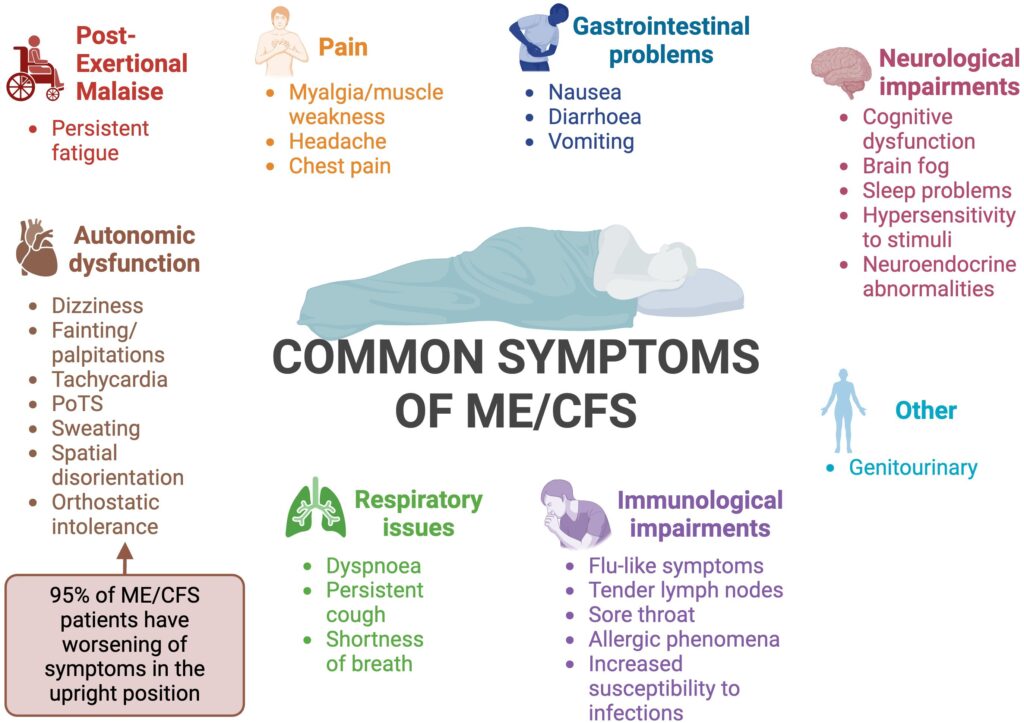
Long COVID & Dysautonomia (ICD10 classified disorder)
Postural Orthostatic Tachycardia Syndrome (Dysautonomia vs POTS)
Stroke Recovery
Concussions & Traumatic Brain Injuries (with specialized concussion therapy near me programs)
Chronic Fatigue & Brain Fog
Neurodegenerative Conditions (Parkinson’s, Early Dementia, Alzheimer’s)
Living with Chronic Migraine & severe headaches
Vertigo & Dizziness
Neurodevelopmental Disorders (ADHD, Autism Spectrum Disorders)

From Dysautonomia and POTS to concussions and chronic migraines, functional neurology chiropractic care offers solutions for a wide range of conditions
Even if those with the diagnoses and symptoms above are told what is wrong, they are often left frustrated that there isn’t a lot that can be done. On the other side, many of these individuals are told that their labs and imaging are normal, often leading to them being sent to a mental health provider.
If you’ve experienced this and have been told your tests are “normal” but you still struggle with symptoms, functional neurology may be the missing piece in your health journey.
How Does Functional Neurology Differ from Traditional Neurology?
One of the biggest misconceptions in healthcare is that there is only one approach to evaluating and treating the nervous system. In reality, traditional neurology and functional neurology take completely different approaches:
| Traditional Neurology | Functional Neurology |
| Focuses on disease pathology and structural damage | Focuses on neurological function and performance |
| Relies on imaging (MRI, CT scans) and blood work | Uses in-depth neurological testing (eye movements, balance, cognitive function, QEEG) |
| Treatments focus on medications and surgery | Treatments involve targeted brain rehabilitation and neuroplasticity training |
| Often tells patients “there’s nothing wrong” if no pathology is found | Identifies and corrects neurological dysfunctions even if imaging is normal |
Both of these approaches to brain health and function have a place as neither one is equipped to handle all neurological-based symptoms and conditions.
Many patients leave traditional neurology appointments feeling unheard, frustrated, and stuck with no solutions. Functional neurology changes the game by addressing how the brain functions and finding ways to restore it. That’s why so many patients now seek out a dedicated center for community brain health like Peak Brain and Body.
What to Expect in a Functional Neurology Evaluation
At Peak Brain and Body, a functional neurology evaluation is a deep dive into your brain’s function, using the latest advanced neurological testing that most doctors don’t even know exist. These evaluations include:
1. Eye Movement Analysis (Video Oculography)
Your eye movements provide a direct window into your brain health. Using cutting-edge videooculography, we can detect dysfunctions in different areas of the brain, helping guide targeted rehabilitation.
2. Balance & Postural Testing (Computerized Balance Posturography)
A specialized computerized balance platform is used to assess postural stability and vestibular function. Poor balance can be an early indicator of neurodegenerative diseases and cognitive decline. Balance is also routinely off with long-covid, concussions, whiplash, strokes, dysautonomia, and postural orthostatic tachycardia syndrome.
3. Quantitative EEG (QEEG) Brain Mapping
A QEEG measures brain wave activity to identify abnormalities in neural communication, helping tailor treatments for patients with conditions like brain fog, anxiety, PTSD, ADHD, and post-concussion syndrome.
4. Cognitive & Reaction Time Testing
By evaluating how quickly and accurately your brain processes information, we can detect subtle impairments in cognitive function before they become major issues.
5. Functional Neurological Exam
This involves assessing reflexes, coordination, dual-tasking abilities, and cranial nerve function, which reveals how different brain regions are communicating and working together.
Functional Neurology Treatments: Rewiring the Brain for Healing
Once dysfunctions are identified, the next step is highly targeted brain rehabilitation. Unlike protocol-based care, functional neurology chiropractic treatment at Peak Brain and Body is about precision—designing a program based on your brain’s unique weaknesses and strengths.
Common Functional Neurology Treatments Include:
- Oculomotor Therapy – Strengthening brain function by using a specific combination of eye movements.
- Vestibular & Balance Training – Restoring vestibular and cerebellar function to improve dizziness, vertigo, and coordination.
- Hand-Eye Coordination & Reaction Time Exercises – Enhancing cognitive flexibility and neural processing speed.
- Transcranial Magnetic Stimulation (TMS) – A non-invasive therapy that stimulates brain activity and helps depression, anxiety, insomnia, and much more.
- Neuromodulation & Brainwave Training – Using neurofeedback and light therapy to retrain the brain.
- Targeted Physical Exercise – Driving neurogenesis (new brain cell growth) and angiogenesis (new blood vessel formation) to optimize brain function to support treatments performed in the office.
The Evolution of Functional Neurology: Beyond Rehab
Early functional neurology focused primarily on rehabilitation, but the field has expanded to address the broader factors influencing brain health. At Peak Brain and Body, Dr. Zimmerman integrates functional medicine into his neurological treatments, ensuring that underlying factors such as gut health, inflammation, hormones, immune function, and metabolic issues are addressed alongside neurological rehabilitation.
This whole-body approach ensures that patients get the highest level of care and long-term success that functional neurology on its own may not achieve.
Why Patients Travel from Across the Country to See Dr. Zimmerman
Patients don’t just come from Tampa Bay—they fly in from all over the United States and beyond because of Dr. Zimmerman’s expertise, advanced diagnostic techniques, and groundbreaking treatment protocols. For those searching for a traumatic brain injury treatment center that looks beyond standard care, Peak Brain and Body stands out as a trusted leader.
Is Functional Neurology Right for You?
If you have been struggling with brain fog, dizziness, chronic fatigue, memory loss, headaches, concussions, or other neurological symptoms and have been told “everything is normal or nothing else can be done and you must wait it out,” functional neurology may be the answer you’ve been looking for.
At Peak Brain and Body, we go beyond symptom management—we uncover and correct the root cause of neurological dysfunction to help you regain control of your brain and body.
Schedule a consultation with our Peak Brain and Body team today. Don’t wait for answers—get the care you deserve at a leading Tampa Bay functional neurology center.
Is functional neurology the same as chiropractic care?
No, functional neurology is not the same as traditional chiropractic care. While both may address the nervous system, functional neurology focuses specifically on brain function, neuroplasticity, and customized neurological exercises, whereas chiropractic care primarily deals with spinal alignment and musculoskeletal adjustments.
Does functional neurology treat concussion and brain injuries?
Yes. Functional neurology is commonly used in concussion and traumatic brain injury (TBI) recovery. Through neuro-rehabilitation exercises, visual-vestibular therapy, and brain stimulation, patients often experience improvements in focus, balance, memory, and overall brain health.
What conditions can a functional neurology center in Tampa treat?
Functional neurology can help with migraines, vertigo, balance disorders, concussions, ADHD, post-stroke rehabilitation, dysautonomia, POTS, brain fog, and many other neurological challenges.
Is functional neurology safe for long-term treatment?
Functional neurology is considered safe because it uses non-invasive, drug-free therapies. Treatments are customized for each patient and adjusted based on progress, making it a sustainable long-term approach to managing neurological conditions.